Breast Cancer Hormone Receptor Status
Breast cancer cells taken out during a biopsy or surgery will be tested to see if they have certain proteins that are estrogen or progesterone receptors. When the hormones estrogen and progesterone attach to these receptors, they stimulate the cancer to grow. Cancers are called hormone receptor-positive or hormone receptor-negative based on whether or not they have these receptors . Knowing the hormone receptor status is important in deciding treatment options. Ask your doctor about your hormone receptor status and what it means for you.
Evidence Supporting A Limited Role Of Adjuvant Chemotherapy In Hormone
The International Breast Cancer Study Group trial IX randomized 1715 postmenopausal women with lymph node-negative early breast cancer to tamoxifen for 5 years with or without chemotherapy, which consisted of three cycles of classical CMF . Randomization in that study was stratified by ER status, resulting in 23% of patients with ER-negative disease. The overall results of the trial confirmed that three courses of CMF improved disease-free survival significantly. However, analyzing the two subsets based on the status of ER , three cycles of CMF added to tamoxifen had a significant impact on both disease-free and overall survival only in ER-negative patients, with virtually no effect in the ER-positive subset .
| q3 weeks versus q2 weeks doxorubicin, cyclophosphamide and paclitaxel | 7% for q2 weeks versus q3 weeks | 9.1% for q2 weeks versus q3 weeksa | 2.8% for q2 weeks versus q3 weeksa |
HR, hormone receptor DFS, disease-free survival HD, high dose ID, intermediate dose LD, low dose.
aTest of interaction of HR status and efficacy of the experimental regimen were statistically significant.
Characteristics Of Hr+ Advanced Breast Cancer Cohort By Age Groups
The study population for this analysis consisted of 2,342 HR+ ABC patients, with the median age of 49 years and a mean age of 48.97 years. Among the study population, 1,364 patients were diagnosed below 50 years and 978 patients over 50 years. Table 1 summarized the frequency and proportion of some characteristics of these patient groups. There were a series of significant differences among the cohorts of patient samples including PgR status, bone-only metastasis, and visceral metastasis . It was noticed that younger patients had obviously higher rate of PgR positive and bone-only metastasis in our study. On the contrary, elder group tended to have visceral metastasis than younger patients . However, there were no significant differences in histological grade, ER status, HER2 status, metastases-free interval , brain metastasis, and number of metastatic sites among the two age groups . As the leading composition of adjuvant treatment, adjuvant ET was applied to 1,882 patients, of which 976 received selective estrogen receptor modulators and 261 received aromatase inhibitors .
Table 1 Characteristics of patients with HR+ ABC by age group.
Also Check: How To Lower Estrogen In Women
Possible Side Effects Of Ais
The most common side effects of AIs are:
- Hot flashes
- Bone and joint pain
- Muscle pain
AIs tend to have side effects different from tamoxifen. They don’t cause uterine cancers and very rarely cause blood clots. They can, however, cause muscle pain and joint stiffness and/or pain. The joint pain may be similar to a feeling of having arthritis in many different joints at one time. Options for treating this side effect include, stopping the AI and then switching to a different AI, taking a medicine called duloxetine , or routine exercise with nonsteroidal anti-inflammatory drugs . But the muscle and joint pain has led some women to stop treatment. If this happens, most doctors recommend using tamoxifen to complete 5 to 10 years of hormone treatment.
Because AIs drastically lower the estrogen level in women after menopause, they can also cause bone thinning, sometimes leading to osteoporosis and even fractures. If you are taking an AI, your bone density may be tested regularly and you may also be given bisphosphonates or denosumab , to strengthen your bones.
Types Of Hormone Receptors
- There are two types of receptors, estrogen, and progesterone.
- If your tumor has estrogen receptors, it is called estrogen receptor-positive or ER+.
- If your tumor has progesterone receptors, it is progesterone receptor positive or PR+.
- Your tumor can be positive for one or both hormone receptors. This may be written ER/PR+, ER+/PR-, ER-/PR+.
- HR+ breast cancer can also be HER2 positive.
Also Check: What Hormone Makes You Break Out
Benefits Of Hormone Therapies In Early And Locally Advanced Breast Cancer Treatment
Treatment with the hormone therapies tamoxifen and/or an aromatase inhibitor lowers the risk of :
- Breast cancer recurrence
- Breast cancer in the opposite breast
- Death from breast cancer
Premenopausal women who get ovarian suppression plus tamoxifen or an aromatase inhibitor may lower these risks more than premenopausal women who get tamoxifen or an aromatase inhibitor alone .
Learn more about tamoxifen.
|
Aromatase inhibitor plus androgen deprivation therapy |
Surgery To Stop The Ovaries From Working
This is also a type of ovarian ablation. You might choose to have an operation to remove your ovaries instead of having drug treatment to stop them working. You have this operation as keyhole surgery. It is called laparoscopic oophorectomy and you have it under general anaesthetic . You usually stay in hospital overnight.
The surgeon makes a number of small cuts into your tummy . They put a long bendy tube called a laparoscope into one of the cuts. The laparoscope connects to a video screen.
The surgeon puts small instruments through the other cuts to carry out the operation and remove the ovaries. They close the cuts with stitches and cover them with small dressings.
Removing your ovaries causes you to have a sudden menopause. The symptoms include hot flushes, sweating and mood swings.
Read Also: What Are The Different Types Of Hormone Replacement Therapy
Selective Estrogen Receptor Response Modulators
Selective estrogen receptor response modulators attach to and block estrogen receptors in breast cells. This stops the estrogen from signaling to the cells to grow.
Examples of SERMs include:
- toremifene for people with advanced ER-positive breast cancer after menopause
A doctor may prescribe one of these drugs with another medication.
Side effects
Possible adverse effects of SERMs include:
- changes in mood
- vaginal dryness or unusual discharge
Less commonly, SERMs may increase the risk of:
- uterine cancer
from the age of 5074. Those aged 4049 years should ask their doctor about whether screening is a good idea.
Other organizations have different recommendations. For example, the ACS recommends annual breast screenings for females aged 4554 years .
However, each persons situation is different. A doctor may recommend a different screening schedule for someone with a higher risk of breast cancer.
The outlook for people with ER-positive breast cancer tends to be good, especially when a doctor diagnoses it early.
A person with an early diagnosis of any type of breast cancer has a 99% chance of living for at least another 5 years, and often longer, the ACS reports.
However, if the cancer has spread to other organs, the chance of surviving for at least another 5 years is 29%, it notes.
Taking these steps may ultimately lead to a better outlook if a person develops breast cancer:
What Are Hormones And Hormone Receptors
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and in men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
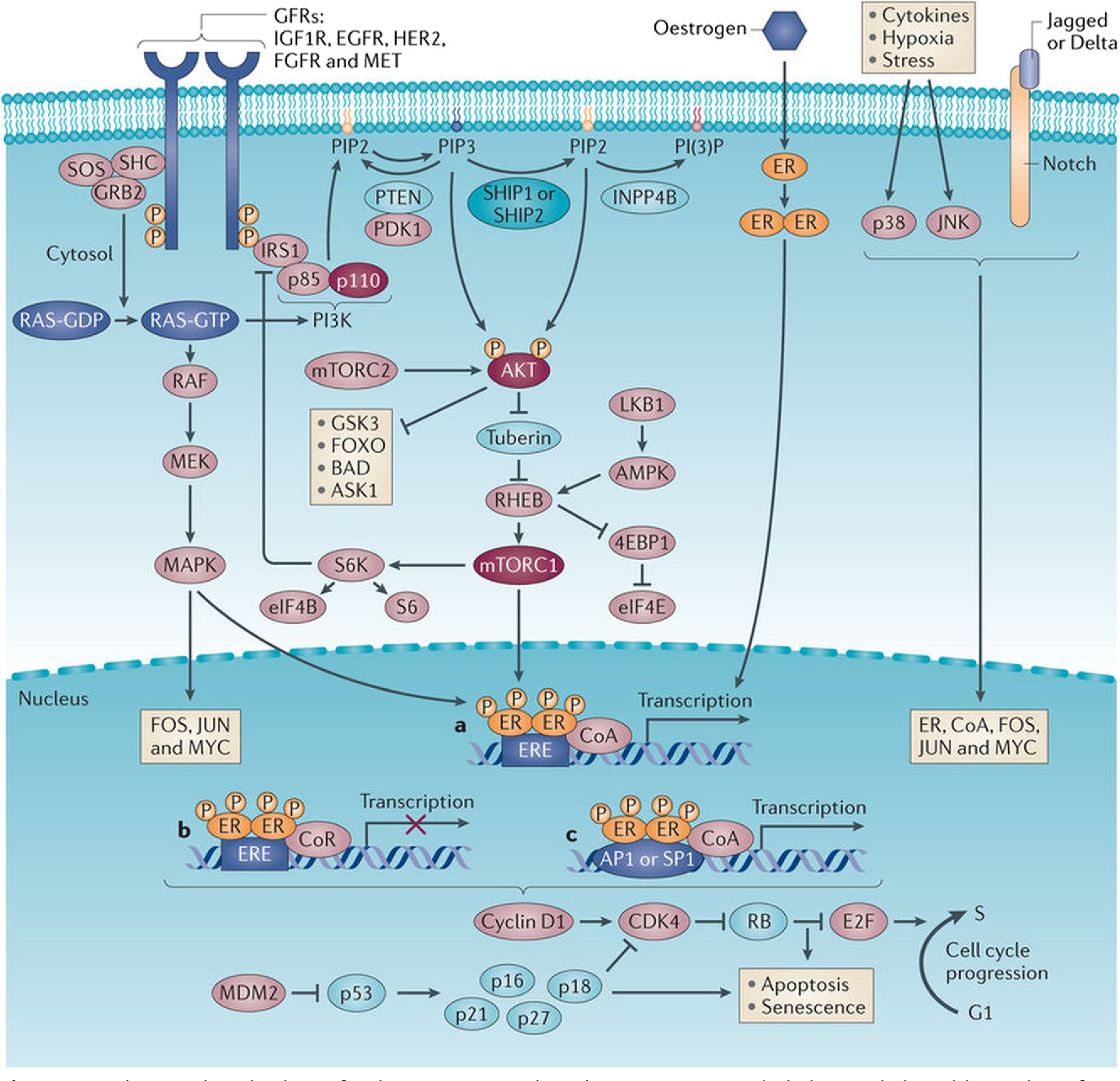
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive breast cancers. Hormone-sensitive breast cancer cells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
Breast cancers that lack ERs are called ER negative, and if they lack both ER and PR they may be called HR negative.
Approximately 67%80% of breast cancers in women are ER positive . Approximately 90% of breast cancers in men are ER positive and approximately 80% are PR positive .
You May Like: What Are Estrogen Rich Foods
If Cancer Comes Back Or Has Spread
AIs, tamoxifen, and fulvestrant can be used to treat more advanced hormone-positive breast cancers, especially in post-menopausal women. They are often continued for as long as they are helpful. Pre-menopausal women might be offered tamoxifen alone or an AI in combination with an LHRH agonist for advanced disease.
Role Of Hormones In The Body
Our bodies naturally make hormones, including estrogen and progesterone.
Estrogen has multiple roles. It helps sex organs develop, makes pregnancy possible, strengthens bones, and more.
As you get older, the level of estrogen in your body changes.
- In women who have periods, the ovaries make most of the bodys estrogen. Estrogen levels in premenopausal women are usually high.
- In perimenopause, the ovaries slow down and make less estrogen. But it is still possible to have menstrual periods, even when the ovaries are working more slowly. Periods may sometimes be irregular. This in-between time happens several years before .
- In menopause, the ovaries gradually stop making estrogen. Periods become irregular and then stop altogether.
- Post-menopausal means a woman has not had any menstrual periods for 12 months in a row and blood work demonstrates hormonal levels are in post-menopausal range.
After menopause, the ovaries no longer make , the most active form of estrogen. But a womans body still makes estrone, another form of estrogen, after menopause. Estrone is made when an enzyme called aromatase converts the male sex hormone androstenedione made in the adrenal glands, ovaries, and fat cells into estrogen. In men, androstenedione is made in the testes.
Don’t Miss: How To Lose Weight With Estrogen Dominance
Hormone Receptor Positive Breast Cancer
Your breast cancer may be hormone receptor-positive or HR+. Some breast cancers have receptors on them that attach to the hormones, estrogen, and progesterone, as they circulate in your body. These hormones feed the cell and help it grow.
- If your tumor has hormone receptors, it is called hormone receptor-positive or HR+. If your tumor is HR+, the tumor needs estrogen and/or progesterone to grow.
- About 80% of breast cancers are HR+.
- If your tumor does not have hormone receptors, it is hormone receptor-negative or HR-.
Guideline Recommendations And Clinical Use Of Genomic Assays
The available gene expression assays vary with regard to the information they provide and the specific patient populations used for assay validation, requiring careful interpretation of results. Uncertainty also remains regarding the applicability of these assays in certain patient populations, including patients who have small tumors and lower-risk clinical features. Despite the limitations of current gene expression assays, genomic testing provides additional prognostic information and is likely superior to basing adjuvant treatment decisions on anatomic staging alone. Breast cancer guidelines from the National Comprehensive Cancer Network , the ASCO, and the ESMO recommend the use of gene expression assays in patients with HR-positive, HER2-negative early breast cancer who have 0 to 3 positive lymph nodes to assess the risk of recurrence and inform decisions regarding the use of adjuvant chemotherapy., , Current guidelines do not emphasize any specific genomic assay over another, and there is significant regional variability in the selection and use of these assays, with each institution often having a preferred test they use most often.
Don’t Miss: How To Correct Hormonal Acne
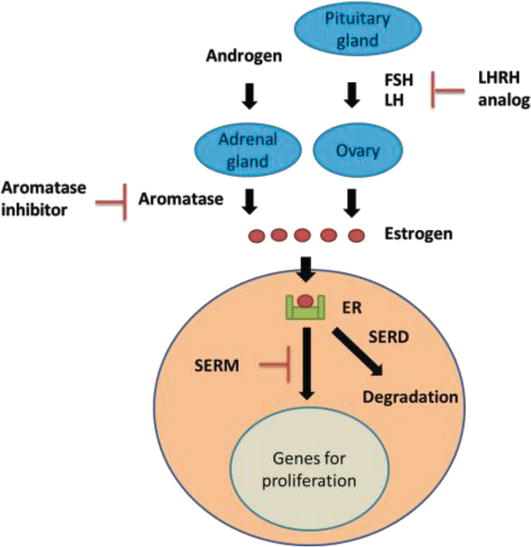
Selective Er Modulators And Down
Tamoxifen is the drug most extensively used when an ET is required, both in pre- and postmenopausal women, and is still considered the SERM of choice. TAM 1A) was initially studied as anti-fertility drug, demonstrating soon favorable effects in patients with ER+ BC, as well as on bone tissue and cardiovascular system. TAM acts as a partial nonsteroidal agonist in some tissues, such as liver, uterus and bone, but is a competitive receptor inhibitor in the breast and brain. In these tissues, TAM selectively blocks signaling at the level of ERs, also inhibiting the proliferation of ductal cells. TAM is hydroxylated by the cytochrome P450 enzyme system into 4-hydroxy tamoxifen , and further metabolized in the liver, thanks to a CYP2D6-mediated oxidation, to endoxifen . Endoxifen and 4HT are the main active metabolites of TAM, exhibit similar ability in binding to ERs, and are more potent than TAM in suppressing estrogen-dependent cancer cells. The relationship between CYP2D6, endoxifen or 4HT serum levels and the response to TAM therapy has long been studied, but the hypothesized role of CYP2D6 genotype as prognostic factor affecting recurrence in patients with BC was not confirmed. However, CYP2D6 inhibitors, such as antipsychotic drugs, selective serotonin reuptake inhibitors , and some cardiac medications have the potential to affect response to SERM therapy.
Chemical structures of the main selective estrogen receptor modulators.
Testing For Hormone Receptor
After a breast cancer , the removed sample of breast is sent to a lab for testing. If the tissue is confirmed to have cancer cells, the tests help your care team learn more about the cancer and how to treat it. Your doctor will share the test results with you in a document called a pathology report.
One test performed on breast cancer cells is called an immunohistochemical staining , or IHC test. This test checks the hormone receptor status of the cancer cells. IHC tests show whether the cancer cells have estrogen receptors, progesterone receptors, or both.
Read Also: What Foods Help With Hormonal Acne
If You Cant Have Surgery
Surgery is the main treatment for breast cancer, but some women have health problems that mean they cant have surgery. Some women choose not to have surgery.
In this case, if your breast cancer is oestrogen receptor positive, your doctor might recommend hormone therapy. This treatment won’t get rid of the cancer but can stop it growing or shrink it.
The treatment can often control the cancer for some time. Your doctor might change you to a different type of hormone treatment if your cancer starts growing again.
What Hormone Receptors Do
Hormone receptors, like other cell receptors, are special proteins found in and on the surface of certain cells throughout the body, including breast cells. These receptor proteins are like the eyes and ears of the cells, receiving messages from hormones and other substances in the bloodstream and then telling the cells what to do. The receptors act like an on-off switch for an activity in the cell. If the right substance comes along that fits into the receptor like a key fitting into a lock the switch is turned on and that particular activity in the cell begins.
Read Also: Does Melatonin Come In Liquid Form
What Do The Hormone Receptor Test Results Mean
Test results will give you your hormone receptor status. It will say a tumor is hormone receptor-positive if at least 1% of the cells tested have estrogen and/or progesterone receptors. Otherwise, the test will say the tumor is hormone receptor-negative.
Hormone receptor-positive breast cancer cells have either estrogen or progesterone receptors or both. These breast cancers can be treated with hormone therapy drugs that lower estrogen levels or block estrogen receptors. Hormone receptor-positive cancers tend to grow more slowly than those that are hormone receptor-negative. Women with hormone receptor-positive cancers tend to have a better outlook in the short-term, but these cancers can sometimes come back many years after treatment.
Hormone receptor-negative breast cancers have no estrogen or progesterone receptors. Treatment with hormone therapy drugs is not helpful for these cancers. These cancers tend to grow faster than hormone receptor-positive cancers. If they come back after treatment, its often in the first few years. Hormone receptor-negative cancers are more common in women who have not yet gone through menopause.
Triple-positive cancers are ER-positive, PR-positive, and HER2-positive. These cancers can be treated with hormone drugs as well as drugs that target HER2.
Why Should Breast Cancer Be Tested For Hormone Receptors
Every patient with a breast cancer diagnosis undergoes a hormone receptor evaluation that helps determine if the cancer cells have receptors for estrogen and progesterone.
About 2 out of every 3 breast cancer cases test positive for hormone receptors.
Testing breast cancer cells for hormone receptors is important to decide whether hormonal therapy will be an effective course of treatment.
Hormone therapy involves reducing the estrogen levels in the body or blocking the cells from responding to estrogen.
Only if the cancer is ER-positive, hormone therapy will work.
This makes ER-negative cancers difficult to treat non-hormonal treatments are used for these cancers.
Also Check: Are Olly Melatonin Gummies Safe
What Are The Side Effects Of Hormone Therapy
The side effects of hormone therapy depend largely on the specific drug or the type of treatment . The benefits and harms of taking hormone therapy should be carefully weighed for each person. A common switching strategy used for adjuvant therapy, in which patients take tamoxifen for 2 or 3 years, followed by an aromatase inhibitor for 2 or 3 years, may yield the best balance of benefits and harms of these two types of hormone therapy .
Hot flashes, night sweats, and vaginal dryness are common side effects of all hormone therapies. Hormone therapy also may disrupt the menstrual cycle in premenopausal women.
Less common but serious side effects of hormone therapy drugs are listed below.
Tamoxifen
- breathing problems, including painful breathing, shortness of breath, and cough
- loss of appetite
Assessing Recurrence Risk In Patients With Hr
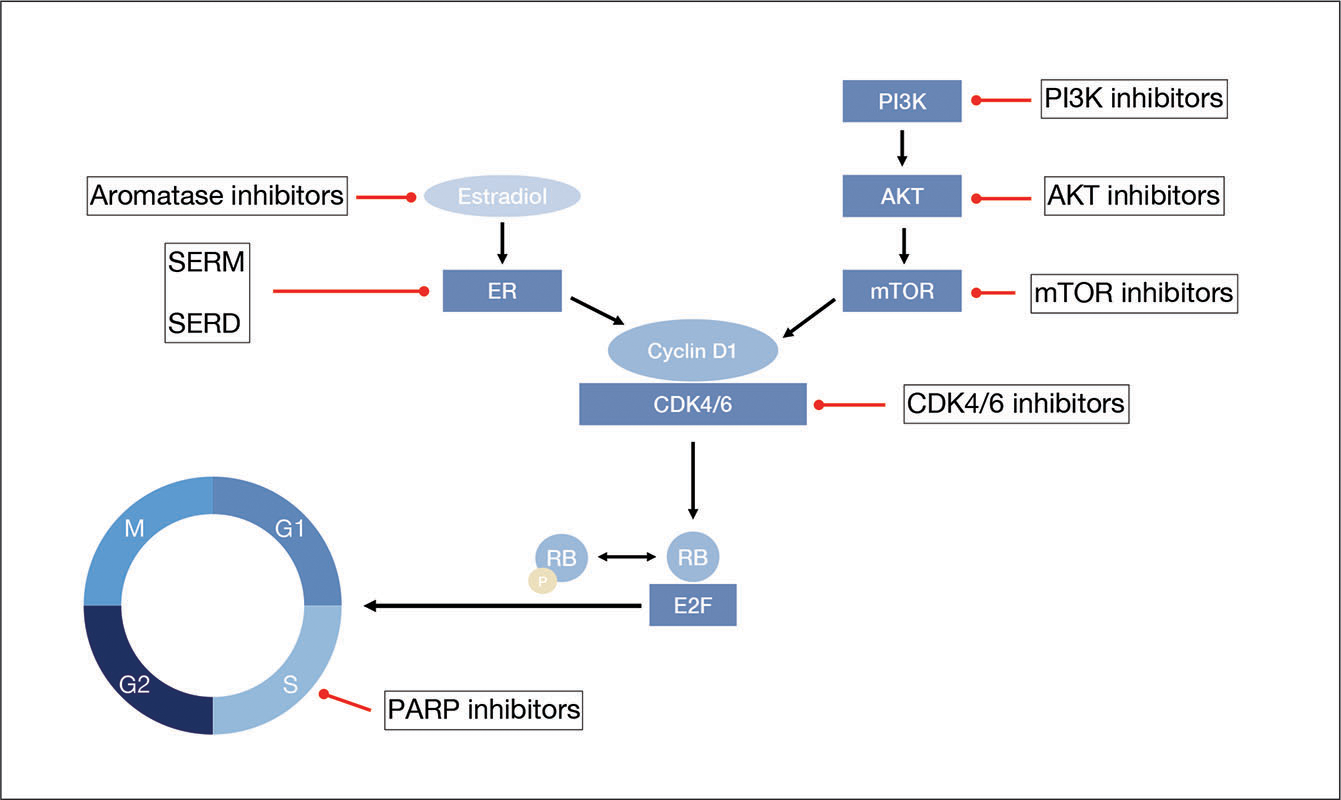
Adjuvant therapy options for HR-positive early breast cancers center on endocrine therapy and chemotherapy. Optimal treatment selection requires an accurate assessment of an individual’s risk for disease recurrence. A higher risk of recurrence and a poorer prognosis are associated with large tumor size, increased numbers of nodes, high histologic grade, and vascular invasion. The staging criteria from the American Joint Committee for Cancer was updated in 2018 to incorporate biologic factors such as tumor grade, estrogen receptor status, progesterone receptor status, HER2 status, and multigene assays.
You May Like: What Testosterone Does To The Body