Pathophysiology Of Hormone Allergy
An enzyme known as cytochrome P-450 1B1 converts 17 -estradiol to 4-HE . Further, numerous enzymes can change 4-HE into compounds called 3,4-semiquinones and 3,4-quinones. Though estrogen, progesterone, and other hormones are present in the body in tiny quantities, hormones are also synthesized directly in cells in target tissues, far exceeding the amount of the hormone in blood, for example, adipose tissues and adrenal tissues. As the tissue itself makes hormone, there is enough present to make high levels of hormone metabolism leading to protein and DNA adducts. While adducts between cellular proteins and hormone metabolites may induce antihormone and anti-tissue antibodies, the DNA-hormone adducts may trigger DNA damage. Hormone adducts are formed by intercalation of steroid hormones between the stacked bases in the DNA, for example, estrogen-DNA adducts .
Impact Of Steroid Hormones On Immunity
The immune system provides a strong defense against internal and external threats. However, factors produced in the microenvironment can either enhance or limit its activity and lead to immunopathology. Steroid hormones alter both innate and adaptive immune processes and steroid hormone receptors are expressed by a variety of immune cell populations, including granulocytes, natural killer cells, monocytes, dendritic cells , and B and T lymphocytes, which can affect disease outcome.1 Many autoimmune/inammatory conditions, such as systemic lupus erythematosus , exhibit gender differences in incidence. This suggests a role for sex hormones in disease development.2 Numerous studies provide evidence for bi-directional communication between the immune and endocrine systems and disruptions in communication that contribute to susceptibility and severity of disease.
Glucocorticoids modulate immunity, and their overall effects depend on dosepharmacologic or physiologicand temporal sequence of release in relation to antigenic or pro-inammatory challenges.3 Stress levels of glucocorticoids result in rapid involution of the thymus and lymphocyte apoptosis. Glucocorticoids also orchestrate redistribution of circulating white blood cells with neutrophilic leukocytosis, eosinopenia, monocyteopenia, and altered ratios of T-lymphocyte subtypes, resulting in decreased peripheral blood CD4+ and increased CD8+ cells and decreased inltration of neutrophils and monocytes into tissues.
What Is Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disorder that causes chronic inflammation in the joints. This happens when the bodys immune system starts attacking itself instead of foreign pathogens, such as bacteria or viruses.
The result is a thickening of the lining inside the joints, causing swelling and pain. Over time, RA can cause a loss of cartilage and bone, as well as joint deformity.
About 1.5 million Americans have RA. Its almost three times more common in women than in men. Women usually develop this disorder between the ages of 30 and 60, and men usually develop it later in life.
RA may also affect more than your joints. Symptoms in other parts of the body may include:
RA can present itself in different ways. However, symptoms are usually symmetrical, meaning they affect the same parts of the body on both sides at the same time. Also, symptoms often come and go.
You May Like: Seed Cycling For Balancing Hormones
Welcome To Celiaccom You Have Found Your Celiac Tribe Join Our Like
Reviewed and edited by a celiac disease expert.Caption:
Celiac.com 05/16/2011 – Nearly 75% of the 24 million Americans suffering from autoimmune disease are women, according to the American Autoimmune Related Diseases Association . Women appear to mount larger inflammatory responses than men when their immune systems are triggered, thereby increasing their risk of autoimmunity. The fact that sex hormones are involved is indicated by the fact that many autoimmune diseases fluctuate with hormonal changes such as those that occur during pregnancy, during the menstrual cycle, or when using oral contraceptives. A history of pregnancy also appears to increase the risk for autoimmune disease.
Celiac.com Sponsor :They based their study on the known data that DHEA not only declines with aging but is reduced in Sjogrens, an autoimmune disease. The study was populated by 23 post-menopausal women with primary Sjogrens syndrome and subnormal levels of DHEA. The investigation was a controlled, double blind crossover study, conducted over a 9 month period, where DHEA was assessed by sophisticated laboratory measurements and typical symptoms of Sjogrens such as dry mouth and eyes and salivary flow rates were similarly assessed.
Results revealed a strong correlation between low DHEA and Sjogrens symptoms. DHEA and its sex hormone metabolites were found to increase with DHEA supplementation but not with the placebo. Symptoms such as dry eyes were seen to improve as estrogen levels
What Are Autoimmune Diseases
An autoimmune disease occurs when your immune system begins attacking your body instead of foreign contagions, such as viruses and bacteria.
The immune system works by marking foreign proteins and then destroying them. However, for those with an autoimmune disease, the immune system mistakenly marks proteins that are a part of you. Then, when the immune system sets out to destroy any marked proteins, it ends up attacking itself.
Sex hormones appear to play a role in autoimmune diseases since these diseases typically fluctuate with hormonal changes. For example, some instances that cause autoimmune diseases to flare up include the menstrual cycle, pregnancy, or using oral contraceptives. All of these instances result in dramatic changes in female sex hormone levels.
Don’t Miss: What Do Melatonin Gummies Do
The Connection Between Androgens And Sle
In the absence of corticosteroids that decrease levels of free testosterone, oxidation of testosterone at C-19 was increased in female patients with SLE.4 Males did not show this metabolic aberration. For many years, the occasional observation of autoimmune disease in hypogonadal males with Klinefelter syndrome or acquired hypogonadism has reinforced the putative link between the absence of androgens and worsened disease in humans. The observation that hormones such as dehydroepiandrosterone could ameliorate the murine illness suggested that this might be useful as a therapy in humans.5 Unfortunately, this was not the case. DHEA therapy of SLE patients did not meet end points in early studies and was abandoned. Use of 19-nortestosterone to treat the disease and avoid aromatization of estrogens was also unsuccessful. Curiously, males who were treated with this steroid had worsened disease, possibly because of feedback inhibition of endogenous testosterone.
What Is Estrogen Dominance
SImply put, estrogen dominance is a hormone imbalance in which estrogen levels are too high in relation to progesterone. Estrogen and progesterone act as a checks and balance system in the body, regulating each others functions. The problem occurs when one is incredibly high or low in relation to the other. This can happen naturally during times of puberty, pregnancy, or menopause, or it can occur due to environmental changes. Estrogen dominance is currently at an all time high, with factors such as diet, environmental toxins, and chronic stress, playing a major role.
Recommended Reading: Average Cost Of Bioidentical Hormones
What Are The Symptoms Of Adrenal Fatigue
Adrenal fatigue symptoms can vary from individual to individual, but there are some common symptoms experienced by almost all. These include insomnia, a feeling of being overwhelmed by stressful situations, food cravings, high levels of fatigue each day, and weak immunity.
These symptoms are mostly related to the changing hormone and neurotransmitter levels that come with Adrenal Fatigue. There are a number of other, less common, symptoms that can also appear. These might include vertical lines on the fingertips, frequent urination, and low blood pressure. Again, these are all related to the dysregulation of the HPA axis and the various hormone levels that depend on it.
Read Also: Best Way To Deal With Sinus Infection
T Cell Differentiation And Cytokine Production
Estrogen regulates a number of cytokines that modulate the immune response. Pharmacologic doses of the synthetic estrogen diethylstilbestrol in mice led to reduced proliferation of splenic T cells, reduced IL-2 production and increased susceptibility to Listeria monocytogenes infection . Estrogen increases NFB signaling activity and its ensuing cytokines including IL-1, IL-10, and IFN- in C57Bl/6 mouse splenocytes . To assess the role of estrogen on T cell immune responses, concentration dependent effects of 17–estradiol in vitro cultures of T cells and splenocytes from rats were studied to assess the effects on proliferation, cytokines , and signaling molecules ERK1/2, CREB, and Akt . Lower concentrations of estrogen enhanced proliferation and IFN- production in an ER dependent manner. The ER agonist propyl pyrazole triol suppressed IL-2, but the ER agonist diarylpropionitrile increased IL-2. These effects were associated with increased levels of phosphorylated -ERK, p-Akt and p-CREB and increased activity of antioxidant enzymes and NO production .
Estrogen increased levels of IL-17 and its driving transcription factor retinoic acid receptor t in activated splenocytes from male and female C57Bl/6 wild-type mice and in lupus-prone male NZB/W mice. IL-27 and IFN- suppressed the IL-17 induction .
Recommended Reading: How To Check If Your Hormones Are Out Of Balance
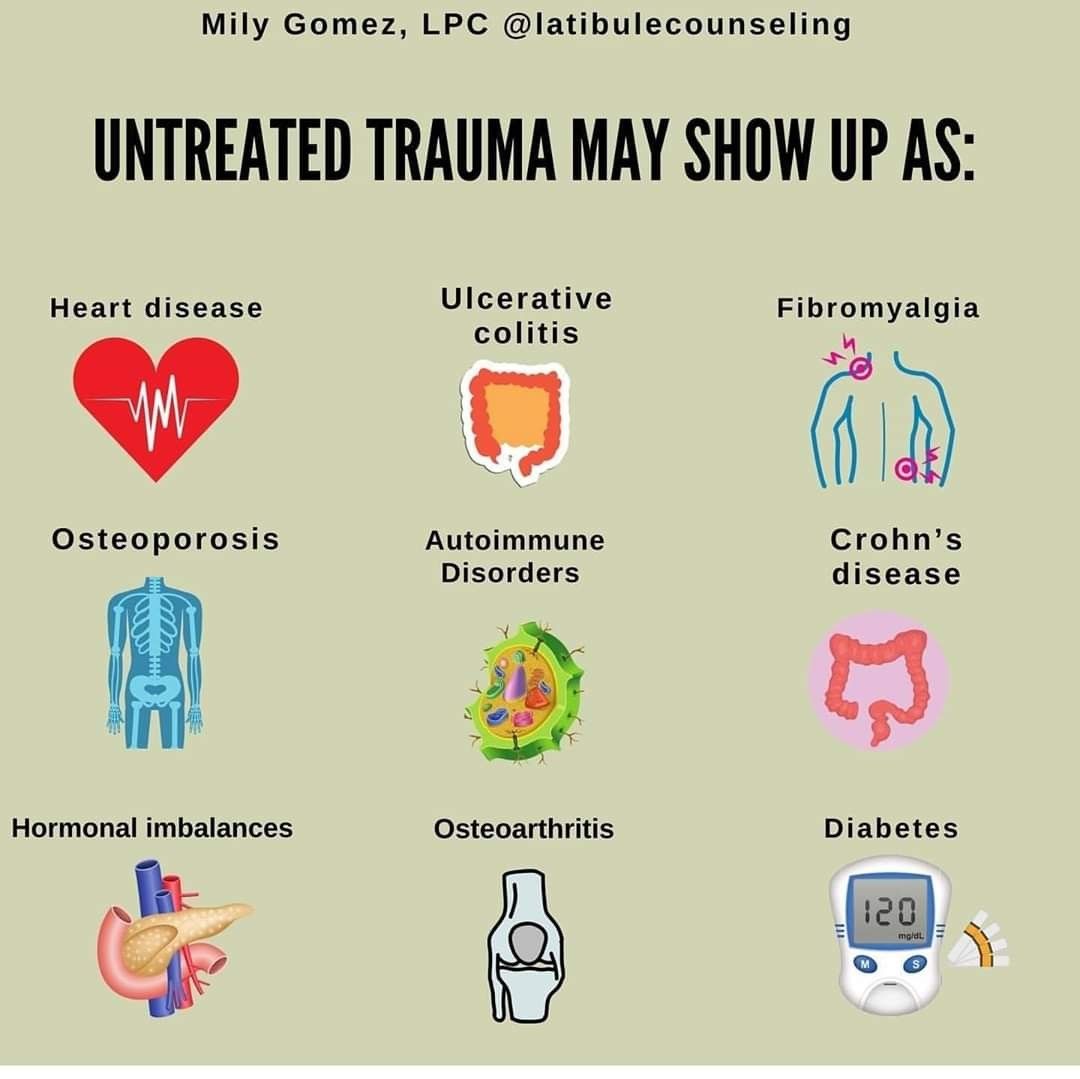
Autoimmune Diseases & Hormone Imbalances In Women
We also find that most autoimmune diseases dont seem to happen individually if you have one, youre at increased risk of developing another. After all, it is your immune system going a bit haywire in the body, so the chance of it impacting other organs/systems/cells in the body is increased. Researchers have even found that sex hormones can have an impact on the genes related to autoimmunity in susceptible people as young as in utero, or shortly after birth. This means that if you have a family history of autoimmune disease, that little increase in sex hormones at the beginning of your life can play a role on developing autoimmune diseases years or decades later in your life.
So what can we do about it? How can we set ourselves up for the most success? If you have an autoimmune disease, what other routes should you consider to get a whole person approach to your care?
Hormones And Autoimmune Disease
Hormonal disorders as well as autoimmune diseases are both on the rise. And who do they effect the most? Women. Studies show that 75% of the patients suffering from autoimmune diseases are women.
But what is the link between the two, if any? Why is it that women are more susceptible to them than men? What precautionary measures can be taken to get rid of this problem? If you have recently been having symptoms that are somewhat like an autoimmune disease or some hormonal issues, here are some things to help.
Don’t Miss: Best Vitamin C Serum For Hormonal Acne
How Does Hormone Health Impact Your Immune System
With all of us trying to stay healthy and avoid getting sick, it seems like everyone is willing to try anything to strengthen their immune system for better protection from disease. Many adopt a healthy lifestyle by eating better and getting more exercise. Others stock up on supplements. And some try getting more sleep. But few people realize that all of these habits may not be enough if your hormones are unbalanced. Thats because your hormones have a direct effect on the strength of your immune system. See, balanced hormones equal better immunity. If youre experiencing hormonal imbalance, its more important than ever to discover the root and the remedy to keep your immune system strong and tip the scales in favor of better health.
The Balancing Act Between Hormones and Your Immunity
So how do your hormones affect your health and your life? Well, hormones are chemical messengers produced by your body that regulate many processes, from your mood and your energy level, to your blood pressure, appetite, sex drive, physical performanceand yes, your immune system. As a result, hormones control how you feel and function.
The Impact of an Imbalance
The hormones that play the biggest role in our health and our quality of life are estrogen, progesterone and androgens like testosterone. As we age, our bodys natural levels of these hormones can drastically fluctuate. This sudden shift can also result from menopause, obesity and other medical conditions.
Dont Get Mad, Get Even
The Cortisol Estrogen Connection
As weve already discussed, elevations in estrogen may drive inflammation and autoimmunity. But it doesnt need to be a frank elevation of estrogen, it can be a relative state of estrogen dominance that contributes to immune dysregulation and many unwanted hormone symptoms.
Cortisol and progesterone share a common precursor hormone called pregnenolone. When stress, inflammation, or immune dysregulation is high, your body will preferentially make cortisol to try to dampen the inflammation. The result is elevated cortisol at the expense of progesterone.
Progesterone naturally opposes estrogen, or in other words, protects you from the harmful effects of estrogen. When progesterone dips estrogen is left unopposed and you experience what is called a relative estrogen dominance.
Now there is lots of cortisol trying to dampen inflammation and lots of estrogen trying to ramp it up. And to make matters worse, you might be resistant to that cortisol. The result? Inflammation climbs and autoimmune disease goes wild!
Read Also: Blood Work For Hormone Panel
The Role Of Female Hormones
When looking at sex hormones, testosterone typically has an immunosuppressive effect, whereas estrogen has an immunoenhancing effect. Just two of the roles of estrogen in the immune system include regulating the immune response and inducing T cells to home in on marked proteins.
Its not just estrogen that impacts the immune system, either, with progesterone helping to inhibit the inflammatory innate immune response.
This shows that female hormones play a vital role in the immune system, and how effectively they accomplish this depends on their concentration in the body.
Appetite And Weight Gain
You may gain weight during hormonal shifts, such as menopause. But hormone changes donât directly affect your weight. Instead, it likely happens because of other factors, like aging or lifestyle. For example, when youâre feeling blue or irritated, as you can be when your estrogen levels drop, you may want to eat more. It can also impact your bodyâs levels of leptin, a hunger-revving hormone.
Recommended Reading: Can A Sinus Infection Be Bacterial
Also Check: How To Lower Estrogen Levels
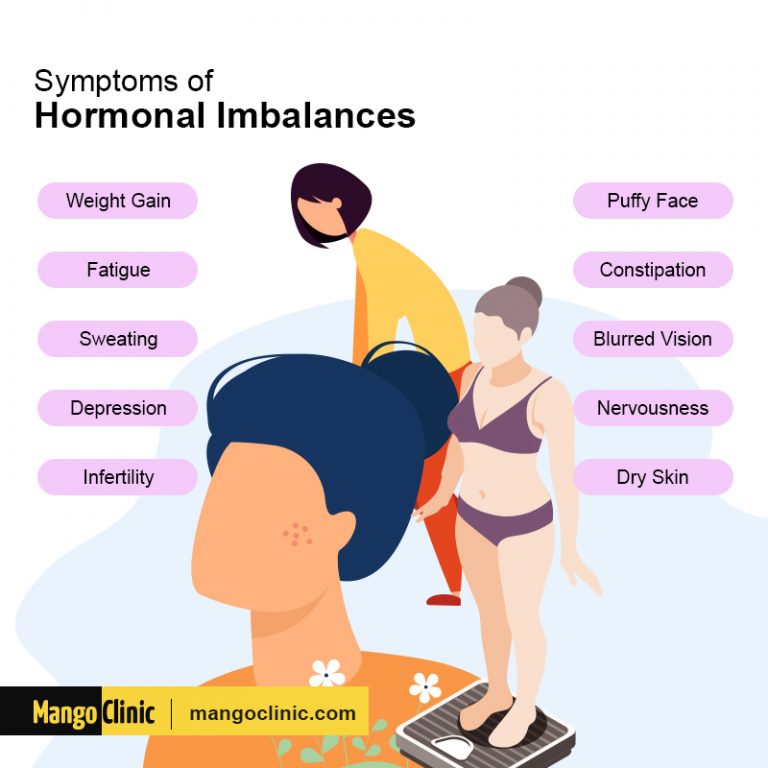
Are These Symptoms Due To Hormone Imbalance
It is easy to brush off symptoms of hormone imbalance and view these as just part of who you are, but really, any symptom reflects something mishappening inside. Here are a few signs to watch for:
- Dry skin, hair and nails
- Feeling the cold
- And just not feeling quite right in yourself
Do any of these sound familiar? If so, it might be worth exploring whether you have a hormonal imbalance.
Next, lets look at the link between specific hormones and autoimmune diseases.
Natural Ways To Balance Your Hormones
Most natural remedies for hormonal imbalance in females can be found in widely available supplements. Many people also experience relief from certain lifestyle changes, including:
- Managing weight
- Getting enough sleep
Hormones have a great role in many processes in our bodies. As weve seen, disruptions of these hormones can cause a variety of symptoms. Sometimes, a hormonal imbalance can have several serious effects. If you seek treatment as soon as possible, youll have the best chance of managing any complications.
References
You May Like: Where Can I Get Bio Identical Hormones
What Is The Connection Between Estrogen And Autoimmunity
Much research has been done in recent years exploring the connection between estrogen and autoimmune diseases. One conclusion we can make is that when estrogen levels become imbalanced, they stimulate inflammation in the immune system, leading to more antibody production.
Why is it that higher levels of estrogen creates more antibodies? Good question. The reason for this increased activity is to create a higher immune response that protects the body against invaders during a womans reproductive years. However, too much estrogen in relation to progesterone can cause antibodies to attack its own tissues, rather than the invaders its supposed to. But why would your body seemingly betray you out of nowhere? Understanding how an autoimmune disease develops is the first step to reversing your symptoms. I talk more about the 3 factors that contribute to autoimmune disease here.
One thing is for sure, this overstimulation of the immune system is a leading cause in developing an autoimmune condition, or worsening an existing one.
For women, balancing estrogen production may be a key component to reducing their risk of developing an autoimmune condition. Unfortunately, estrogen dominance has become a common occurrence in todays world.
How Do Hormones Affect Ra
Medical experts have been investigating links between RA and hormone levels. For women, maintaining normal levels of the reproductive hormones estrogen and progesterone appear to have a protective effect against RA.
Research on a small group of middle-aged women with RA found that they tended to report fewer joint symptoms during the postovulatory stage of their menstrual cycles and during pregnancy. These events cause the levels of estrogen and progesterone to increase.
Women with RA also reported that their symptoms worsened after childbirth and during the second week of their menstrual cycles when reproductive hormone levels were lowest.
The levels of reproductive hormones in womens bodies decrease with age. Women who are approaching or who have gone through menopause have decreased levels of these hormones. Some researchers believe thats why this group of women experience RA more than any other segment of the population. This is also why some doctors recommend women experiencing menopause begin hormone replacement therapy .
Research suggests that HRT, which involves using a combination of progesterone and oestrogen, can decrease the overall activity of a womans RA.
However, it may increase the intensity of disease flare-ups when they do occur. There are also some possible side effects that include:
- fluid retention
- drugs to slow down the progression of RA
- biologic agents to stop certain parts of the immune system from triggering inflammation
Also Check: Does Hormonal Birth Control Prevent Pregnancy
When Oestrogen Becomes Toxic
Exposure to toxins is a critical driver in the onset of autoimmune diseases. You may think of toxins as pollutants in the environment or pesticides in food, but your body can produce toxic byproducts as well.
In certain situations, a type of oestrogen called estrone can be converted into a compound that plays havoc in your body and DNA. It is theorised that this damage in DNA might contribute to the onset of systemic lupus erythematosus . Autoantibodies reactive against host DNA are detectable in the circulation of most people with SLE. Therefore it could be argued that the immune system targets the DNA due to damage already created by the oestrogen metabolite.
More research is needed to understand the link between oestrogen metabolites and autoimmune disease properly. However, given specific oestrogen metabolites are linked to breast cancer, it is worth knowing your current oestrogen status. There are diet and lifestyle strategies that help prevent a buildup of these harmful metabolites.