Study And Validation Cohorts
Since the establishment of the DBCG in 1977, virtually all diagnostic and treatment units in Denmark have applied DBCG guidelines for diagnostic procedures, surgery, radiotherapy, systemic therapy, and follow-up for early-stage breast cancer. Diagnostic, therapeutic, and follow-up data have been accumulated prospectively in the DBCG registry by the use of standardized forms .
According to the DBCG guidelines, treatment regimens have been recommended according to risk classifications made by standard algorithms. We selected a study cohort and a validation cohort among patients prospectively classified as low risk in the DBCG database. The low-risk classification was assigned to patients with favorable prognostic characteristics who received no systemic adjuvant treatment.
The validation cohort was selected from subsequent DBCG low-risk programs implemented in 1999, 2001, and 2004 . Selection criteria were the same as the study cohort. The only modification was that patients in whom the axillary lymph node status was determined by sentinel node technique could be included if the number of excised lymph nodes was one or more. For the validation cohort, the period of surgery was from July 1, 1998, to June 1, 2005. The exclusion criteria were identical to those applied to the study cohort.
Evaluation Of Immunohistochemical Staining
Positive controls and internal areas of normal breast tissues showed strong and uniform staining of the epithelial cells lining the ducts and lobules with minimal back ground reactivity for various cytokeratins, smooth muscle actin, BRCA-1, E-cadherin and GCDFP. For evaluating EGFR, CerbB2 and p53 immunostaining, a known positive external control was utilized. Two cores were evaluated from each tumor. Each core was scored individually then the mean of the two readings was calculated. If one core was uninformative, the overall score applied was that of the remaining core. Assessment of staining was based on a semiquantitative approach. A modified histochemical score was used which includes an assessment of both the intensity of staining and the percentage of stained cells. For the intensity, a score index of 0, 1, 2 and 3 corresponding to negative, weak, moderate and strong staining intensity was used and the percentage of positive cells at each intensity was estimated subjectively. A final score of 0300 is the product of both the intensity and the percentage. Staining of ER and p53 was evaluated in the nuclei of the malignant cells and scored as positive or negative. An H-score of 0 and 50 were considered as cutoff points for positive staining of ER and rest of the markers, respectively. One observer scored the staining pattern , without previous knowledge of the outcomes on two separate occasions and a good correlation between the results was found.
Proteins For Targeted Cancer Drugs
Testing cancer cells for particular proteins can help to show whether targeted drug treatments might work for your breast cancer.
Targeted cancer drugs are treatments that change the way cells work and help the body to control the growth of cancer.
Some breast cancers have large amounts of a protein called HER2 receptor . They are called HER2 positive breast cancers. About 15 out of every 100 women with early breast cancer have HER2 positive cancer.
Targeted cancer drugs such as trastuzumab can work well for this type of breast cancer. These drugs attach to the HER2 protein and stop the cells growing and dividing.
Also Check: How To Have Your Hormones Checked
Recurrence Of Metastatic Breast Cancer
Metastatic breast cancer is considered a chronic disease, so it doesnt go away and recur.
But in recent years, people under age 50 have seen a particularly strong decline in death rates due to breast cancer, according to the Centers for Disease Control and Prevention .
These declines are due in part to improved screening and treatment for the disease.
There are a few general facts that are helpful to know about breast cancer outlook:
- Breast cancer is the most common cancer diagnosis in the United States, according to the
What Are Estrogen Receptors
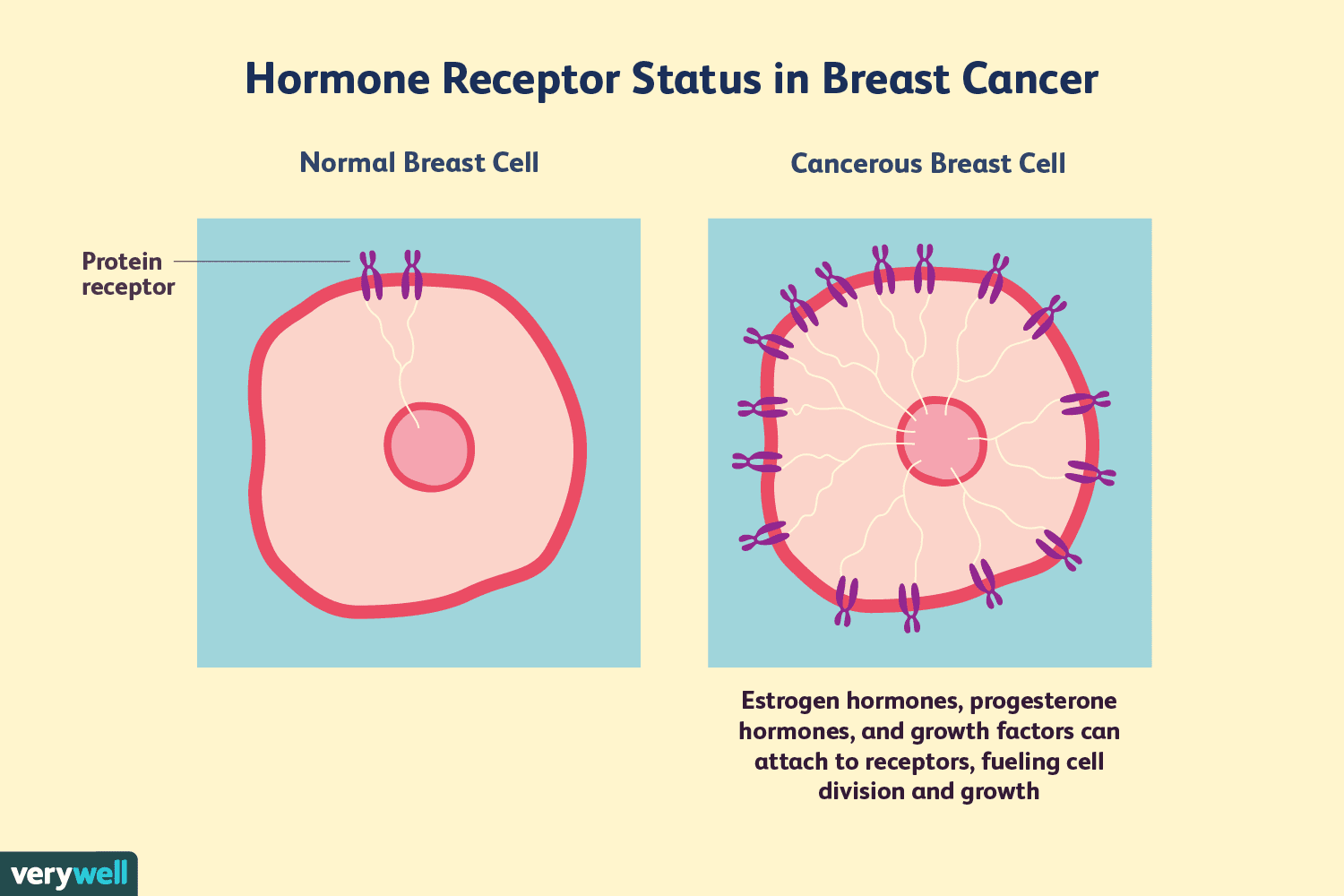
Receptors are proteins inside the target cell or on its surface that receive a chemical signal.
Estrogen is an important hormone responsible for various female characteristics in the body, including the growth and development of breasts .
Estrogen Receptors are a type of steroid receptors that attach to estrogen in the blood and regulate the growth and multiplication of cells in the breast. These receptors pick up signals from the hormones and encourage cell growth.
In the case of breast cancer, this growth is uncontrollable and eventually becomes cancerous.
Recommended Reading: How Much Melatonin Is Good For Sleep
Characteristics Of The Study And The Validation Cohorts
The characteristics of the study and the validation cohorts are shown in . Age at surgery, menopausal status, histopathology group, and ER and/or PR status were similar in the two cohorts. Smaller tumors of 110 mm size were observed more often in patients in the validation cohort compared with patients in the study cohort . Breast-conserving surgery was also noted more often in patients in the validation cohort compared with the study cohort .
Characteristics of low-risk patients in the Danish Breast Cancer Cooperative Group registry with diagnosis of primary invasive breast cancer
Tests On Your Breast Cancer Cells
After a biopsy or surgery to remove breast tissue, a sample of cells is sent to the laboratory. A doctor called a pathologist does various tests on the cells. This can diagnose cancer and also show which type of cancer it is.
Some tests can also show how well particular treatments might work, such as hormone therapies or targeted cancer drugs.
Also Check: How To Find Out Hormone Levels
What Are The Side Effects Of Hormone Therapy
The side effects of hormone therapy depend largely on the specific drug or the type of treatment . The benefits and harms of taking hormone therapy should be carefully weighed for each person. A common switching strategy used for adjuvant therapy, in which patients take tamoxifen for 2 or 3 years, followed by an aromatase inhibitor for 2 or 3 years, may yield the best balance of benefits and harms of these two types of hormone therapy .
Hot flashes, night sweats, and vaginal dryness are common side effects of all hormone therapies. Hormone therapy also may disrupt the menstrual cycle in premenopausal women.
Less common but serious side effects of hormone therapy drugs are listed below.
Tamoxifen
- breathing problems, including painful breathing, shortness of breath, and cough
- loss of appetite
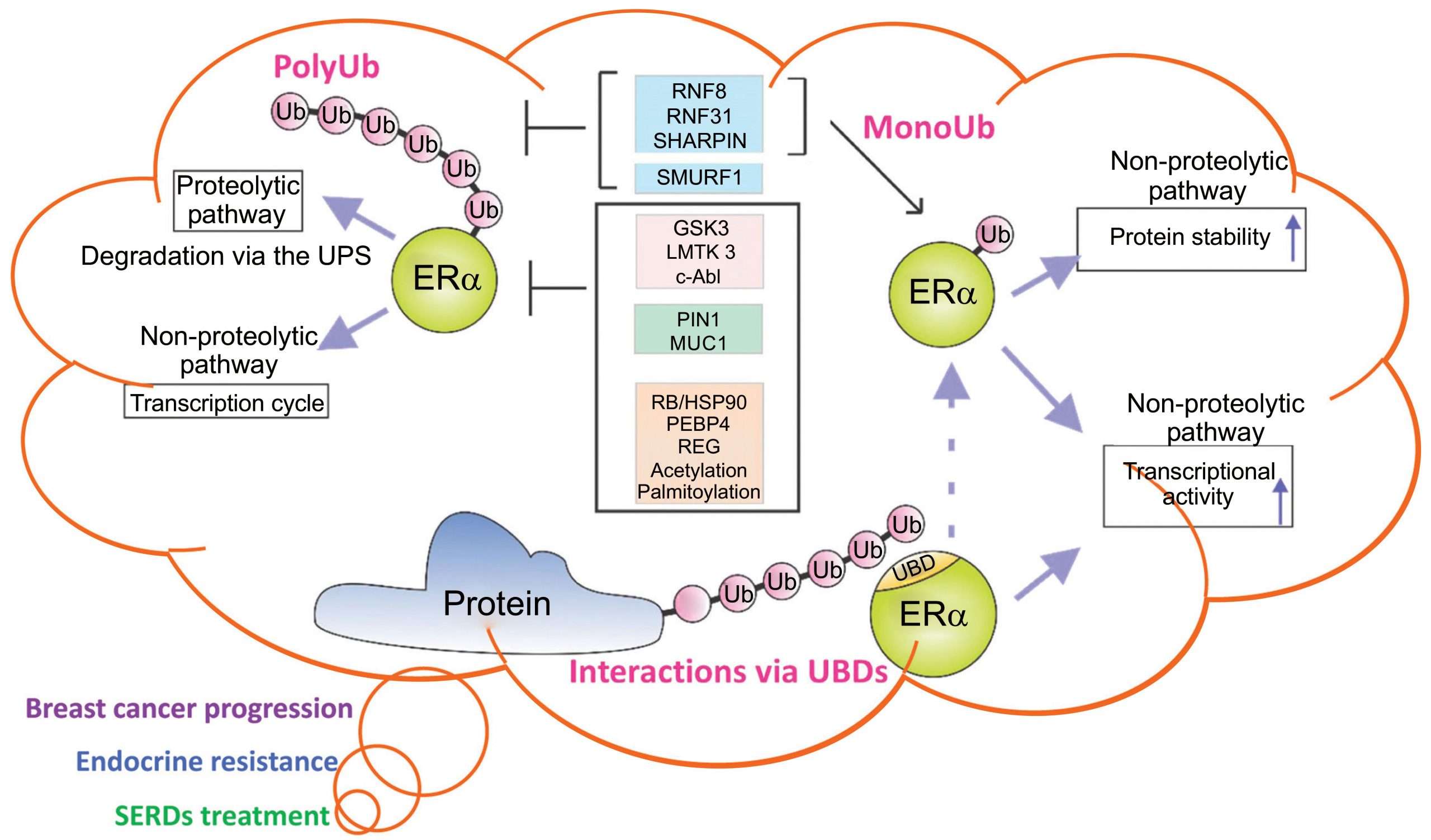
Hormone Therapy For Breast Cancer
Hormone therapy is sometimes used to treat breast cancer. It is a treatment that adds, blocks or removes hormones. Hormones are substances that control some body functions, including how cells act and grow. Changing the levels of hormones or blocking certain hormones can slow the growth and spread of breast cancer cells. Drugs, surgery or radiation therapy can be used to change hormone levels or block their effects.
Hormone therapy is only used for breast cancer that is hormone receptor positive. This means that the cancer cells have receptors for estrogen , progesterone or both. When cancer cells have these receptors, the hormones can attach to them and help them grow. Research has shown that giving hormone therapy after surgery and radiation therapy lowers the risk that the breast cancer will come back, and improves survival.
Breast cancer tissue is always tested to find out if it has hormone receptors or does not have hormone receptors . Find out more about .
You may be offered hormone therapy to:
- lower the risk that non-invasive breast cancer, or may lead to an invasive breast cancer
- lower the risk that invasive breast cancer can come back by destroying cancer cells left behind after surgery and radiation therapy
- shrink a large tumour before surgery
- treat locally advanced or recurrent breast cancer
- relieve pain or control the symptoms of advanced breast cancer
You May Like: What Supplements Help Balance Hormones
Survival Analysis Of Single Hormone Receptor
Approximately 97% of patients with ER + PR- tumors and 88% of patients with ER-PR+ tumors received endocrine therapy. More patients with ER + PR- and ER-PR+ tumors received chemotherapy than the group with ER + PR+ tumors , but less than the group with ER-PR- tumors . Approximately 72% of patients with ER + PR- tumors received both endocrine therapy and chemotherapy, and 24.9% of patients received only endocrine therapy. In ER-PR+ tumors, 80% of patients received both chemotherapy and endocrine therapy, 8.2% of patients received only endocrine therapy and 9.4% of patients received only chemotherapy.
With univariate analysis by Kaplan-Meier method, the survival graph of ER + PR- tumors was located between that of ER + PR+ tumors and ER-PR- tumors. The 5-year and 10-year DFS of ER + PR- tumors was 91.4% and 79.6%, respectively, and the 5-year and 10-year OS was 95.9% and 93.9%, respectively. Patients with ER-PR+ tumors had worse DFS and OS than those with ER + PR-.
Figure 1
Among 1,376 patients with HER2 overexpression, there was no significant difference in DFS between four subgroups , and patients with ER-PR-HER+ tumors had the worst OS . However, the 790 patients who received trastuzumab therapy had similar OS , as did the 586 patients who did not receive trastuzumab therapy .
Figure 2Figure 3Table 2 Multivariate analysis of disease-free survival and overall survival in 1.376 women with HER2-positive breast cancer
Why Your Hormone Status Matters
Breast cancers that are estrogen receptor-positive and/or progesterone receptor-positive are “fueled” by hormones. They’re different from breast cancers that are HER2-positive, in which tumor growth is driven by growth factors that bind to HER2 receptors on the cancer cells. Breast cancers that don’t have any of these receptors are called triple-negative.
Some breast cancers are both hormone receptor-positive and HER2-positive, meaning that estrogen, progesterone, and growth factors can stimulate cell growth. These cancers are often referred to as triple-positive breast cancers.
An ER+ or PR+ score means that hormones are causing your tumor to grow and hormone suppression treatments are likely to work well.If the score is negative , then your tumor is not driven by hormones and your results will need to be evaluated along with other tests, such as your HER2 status, to determine the most effective treatment.
If the only information you’re given is that your hormone status tests are negative, it’s good to ask your healthcare provider for a number that indicates the actual score. Even if the number is a low one, the tumor may effectively be treated with hormone therapy.
Read Also: How Long Does Children’s Melatonin Take To Work
Data Collection And Extraction
The following data from all selected studies was collected independently by two reviewers : year of publication, study design, study population, length of follow-up, assay type and cut-off used, sequence of primer or probe, statistical methods used and reported association between marker and patient outcome were collected from all selected studies. When available, both univariate and multivariate outcome measures were collected. Study population information consisted of population size, country of patient selection, age, grade, hormone receptor status, HER2 status and stage according to the reported American Joint Committee on Cancer classification . The level of evidence was assessed for each publication according to criteria as defined by Hayes et al. and the OCEBM Levels of Evidence Working Group .
For each publication, all study endpoints on outcome were collected and compared with the proposed Standardized definitions for Efficacy EndPoints in adjuvant breast cancer trials . Endpoints not defined in accordance to STEEP definitions were converted to STEEP-defined endpoints when sufficient information was provided. All defined biomarkers were checked for aliases in the NCBI Gene database and were reported by their current RefSeq gene names.
Final Analysis Of Mortality In The Study Cohort After Validation
Final analysis was done to determine the cut points for the continuous risk factors age at surgery and tumor size. Histopathology group was maintained in the model, although the validation analysis showed inconsistent results at 5 years of follow-up. The multivariable analysis of the hierarchical indicator variables showed that increase in age at surgery was associated with decrease in risk of mortality and larger tumor size was associated with an increased risk of mortality. In , relative risk values are presented for the corresponding age and tumor size categories. The categorization of histopathology group was reduced to two levels as follows: histological grade 1 ductal carcinoma and grade 1 and 2 lobular carcinoma vs other or unknown histology. Patients of other or unknown histopathology had a lower relative risk of mortality compared with patients of histological grade 1 ductal carcinoma and grade 1 and 2 lobular carcinoma . For patients of referent histopathology, the relative risk according to age at surgery and tumor size is shown in . The adjusted relative risk of mortality was substantially larger than unity for younger patients aged 3539 years and statistically significantly larger than unity for all patients, except those aged 6074 years with small tumors of 110 mm size .
Cumulative incidence of first disease events in the low-risk study cohort until 10 years after surgery by age at surgery and tumor size
| Age at surgery, y |
Read Also: How Do You Get Your Hormone Levels Tested
What Are Estrogen And Progesterone Receptors
Receptors are proteins in or on cells that can attach to certain substances in the blood. Normal breast cells and some breast cancer cells have receptors that attach to the hormones estrogen and progesterone, and need these hormones for the cells to grow.
Breast cancer cells may have one, both, or none of these receptors.
- ER-positive: Breast cancers that have estrogen receptors are called ER-positive cancers.
- PR-positive: Breast cancers with progesterone receptors are called PR-positive cancers.
- Hormone receptor-positive: If the cancer cell has one or both of the receptors above, the term hormone-receptive positive breast cancer may be used.
- Hormone receptor-negative: If the cancer cell does not have the estrogen or the progesterone receptor, it’s called hormone-receptor negative .
Keeping the hormones estrogen and progesterone from attaching to the receptors can help keep the cancer from growing and spreading. There are drugs that can be used to do this.
Breast Cancer Hormone Receptor Status
Breast cancer cells taken out during a biopsy or surgery will be tested to see if they have certain proteins that are estrogen or progesterone receptors. When the hormones estrogen and progesterone attach to these receptors, they stimulate the cancer to grow. Cancers are called hormone receptor-positive or hormone receptor-negative based on whether or not they have these receptors . Knowing the hormone receptor status is important in deciding treatment options. Ask your doctor about your hormone receptor status and what it means for you.
Also Check: What Are The Negative Effects Of Melatonin
Prospective Ascertainment Of Breast Cancer Cases And The Coding Of Receptor Status
In all countries incident breast cancer cases were identified using record linkage with cancer and pathology registries. In France, Germany and Greece, cancer occurrence was prospectively ascertained through linkage with health insurance records and regular direct contact with participants and their next of kin, and all reported breast cancer cases were then systematically verified against clinical and pathological records. Mortality data were coded according to the 10th Revision of the International Statistical Classification of Diseases, Injuries, and Causes of Death , and cancer incidence data were coded according to the International Classification of Diseases for Oncology . Invasive breast cancer cases were classified as per the International Classification of Diseases for Oncology , second revision . Breast tumor receptor status was standardized across EPIC centers using the following criteria for a positive expression: 10% cells stained, any plus-system description, 20 fmol/mg, an Allred score of 3, an IRS 2, or an H-score 10 .
Vital status was collected from regional or national mortality registries. The last updates of endpoint data for cancer incidence and vital status were between 2005 and 2010, depending on the center. Women were considered at risk from the time of recruitment until breast cancer diagnosis or censoring respectively. A total of 7,095 breast cancer cases had information on ER status of which, 5,843 had further information on PR status .
Risk Of Recurrence: Early And Late
Research has shown the HER2-positive early breast cancers are two to five times more likely to recur than HER2-negative tumors. Even very small HER2-positive tumors with negative lymph nodes have a much higher risk of recurrence relative to tumors that are HER2-negative. Treatment with Herceptin can cut this risk by half.
The pattern of breast cancer recurrence may also differ. Small tumors are also more likely to have a metastatic recurrence if they are HER2-positive.
Despite the fact that HER2-positive and estrogen receptor-negative tuors are more likely to recur early on than estrogen receptor-positive and HER2-negative cancers, late recurrences are much less common.
With estrogen receptor positive breast cancers, the cancer is more likely to recur after five years than in the first five years, and the risk of recurrence remains steady each year for at least 20 years following the diagnosis. In contrast, those who have HER2 positive tumors and reach their five-year mark are much more likely to be “in the clear” and remain recurrence free.
Also Check: How To Control Hormones For Weight Loss
Clinicopathologic Characteristics Of Single Hormone Receptor
The median follow-up duration for the 6,980 patients included in this analysis was 45 months . In this study, 4,651 cases were double HR+ tumors, 1,758 were double HR- tumors, and 571 cases were single hormone-receptor positive tumors, of which 90 cases were ER-PR+ tumors and 481 were ER + PR- tumors. The clinicopathological characteristics of the four subtypes are summarized in Table . Overall, ER+/PR- tumors were found more frequently in postmenopausal women than other subtypes . Compared with ER + PR+ tumor, ER + PR- tumors were not significantly different in staging , but ER+PR- tumors exhibited higher nuclear grade , higher Ki-67 level , and higher EGFR and HER2 expression . However, compared with ER-PR- tumors, ER + PR- tumors showed lower stage , lower NG , lower Ki-67 level , lower p53 expression and lower EGFR expression , but there was no difference in HER2 overexpression .
Table 1 Clinicopathologic characteristics of patients with ER + PR+, ER + PR-, ER-PR+ and ER-PR- tumors
ER-PR+ tumors had higher NG , higher Ki-67 level , and higher expression of p53 and EGFR than ER + PR+ tumors. However, compared with ER-PR- tumors, there was no difference in stage or NG . Also, there was no difference in expression of Ki-67 , p53 , EGFR or HER2 .