Alternatives To Hrt For Protecting Your Bones From Osteoporosis
HRT is no longer recommended for treatment of osteoporosis due to its risks and available alternative options. Bisphosphonate medications are generally recommended to treat osteoporosis instead. Other medications that may be considered are teriparatide, denosumab, or selective estrogen receptor modulators . SERMs are a newer class of drugs, similar to estrogen, that protect against osteoporosis by increasing bone density, while also protecting against the development of breast cancer.
Evista is a widely used SERM that has been shown to increase bone growth and density and reduce the risk of breast cancer. Unfortunately, it does not relieve symptoms of menopause such as hot flashes and may actually worsen them. It is primarily used in women who are at high risk for developing breast cancer or for those who cannot tolerate other medications used to treat osteoporosis.
Additional steps you can take to prevent and/or treat osteoporosis include:
- Performing weight-bearing exercises
What Are The Side Effects Of Hormone Therapy
The side effects of hormone therapy depend largely on the specific drug or the type of treatment . The benefits and harms of taking hormone therapy should be carefully weighed for each person. A common switching strategy used for adjuvant therapy, in which patients take tamoxifen for 2 or 3 years, followed by an aromatase inhibitor for 2 or 3 years, may yield the best balance of benefits and harms of these two types of hormone therapy .
Hot flashes, night sweats, and vaginal dryness are common side effects of all hormone therapies. Hormone therapy also may disrupt the menstrual cycle in premenopausal women.
Less common but serious side effects of hormone therapy drugs are listed below.
Tamoxifen
- breathing problems, including painful breathing, shortness of breath, and cough
- loss of appetite
Hormone Therapy After Surgery For Breast Cancer
After surgery, hormone therapy can be given to reduce the risk of the cancer coming back. Taking an AI, either alone or after tamoxifen, has been shown to work better than taking just tamoxifen for 5 years.
These hormone therapy schedules are known to be helpful for women who are post-menopausal when diagnosed:
- Tamoxifen for 2 to 3 years, followed by an AI for 2 to 3 years
- Tamoxifen for 2 to 3 years, followed by an AI for 5 years
- Tamoxifen for 4½ to 6 years, followed by an AI for 5 years
- Tamoxifen for 5 to 10 years
- An AI for 5 to 10 years
- An AI for 2 to 3 years, followed by tamoxifen for 2 to 3 years
- For women who are unable to take an AI, tamoxifen for 5 to 10 years is an option
For most post-menopausal women whose cancers are hormone receptor-positive, most doctors recommend taking an AI at some point during adjuvant therapy. Standard treatment is to take these drugs for about 5 years, or to take in sequence with tamoxifen for 5 to 10 years. For women at a higher risk of recurrence, hormone treatment for longer than 5 years may be recommended. Tamoxifen is an option for some women who cannot take an AI. Taking tamoxifen for 10 years is considered more effective than taking it for 5 years, but you and your doctor will decide the best schedule of treatment for you.
These therapy schedules are known to be helpful forwomen who are pre-menopausal when diagnosed:
You May Like: Hormone In The Endocrine System
Tumor Characteristics And History Of Mht Use
Lower grade tumors and lobular type breast cancers were more common in the group who had ever used MHT vs. the group who had not. Ever MHT users had a higher tendency to have ER+ tumors compared with never MHT users. Some differences in grade III and ER status along with similar tumor size and nodal status imply that the tumors in ever MHT users were somewhat less aggressive .
Hormone Therapy For Breast Cancer
Some types of breast cancer are affected by hormones, like estrogen and progesterone. The breast cancer cells have receptors that attach to estrogen and progesterone, which helps them grow. Treatments that stop these hormones from attaching to these receptors are called hormone or endocrine therapy.
Hormone therapy can reach cancer cells almost anywhere in the body and not just in the breast. It’s recommended for women with tumors that are hormone receptor-positive. It does not help women whose tumors don’t have hormone receptors .
You May Like: What Can I Take To Increase My Testosterone
Breast Cancer Incidence By Type And Age Over Time
Between 2002 and 2014, a total of 14,085 breast cancer cases were identified among MHS female members age20. These cases included 12,354 patients with invasive breast cancer and 1731 patients with in-situ breast cancer . The median age at diagnosis for those with invasive breast cancer was 56.0 and 54.0 for those diagnosed with in-situ breast cancer. The age-adjusted incidence rate of invasive breast cancer peaked in 2005 and decreased thereafter . The decline for overall breast cancer and for invasive breast cancer was significant for the 20022014 period. EAPC was 0.88 overall, 0.94 for invasive breast cancer and 0.36 for in situ breast cancer. Age is a risk factor for breast cancer overall , and for invasive and in situ breast cancer separately . In women age 5074, for whom biennial mammography tests are routinely performed at a subsidized price, as part of the national screening program for breast cancer, the invasive breast cancer incidence peaked around 2005, consistent with the mammography increase that year , and declined thereafter . In patients, age75 years, for whom mammography screening is not routinely performed, no such peak was observed .
Breast cancer incidence 20022014. Age-adjusted annual incidence rate of breast cancer by type and overall. Age-specific annual incidence rates of breast cancer overall .
Strengths And Weaknesses In Relation To Other Studies
Our study used a nested case-control design, so it did not follow women prospectively from the start of HRT or assess average lifetime risks. Rather, it looked back at already recorded exposures to HRT for women with a diagnosis of breast cancer and matched controls in the age range 50 to 79 and produced comparisons of risks averaged across all time points at which diagnoses in the datasets occurred. The study is based on data derived from real world treatment settings, when women might not have had a constant supply of a preparation and might have needed to switch drugs during the study period. Including all exposures prescribed over time allowed us to present information for a wide range of common types of HRT.
Most trials produced results for a more restricted number of treatments. A meta-analysis of existing trials,7 taken largely from the Womens Health Initiative study, provided estimates only for the specific treatments of conjugated equine oestrogen with and without medroxyprogesterone.6 In contrast to our estimates of a slightly increased risk for long term users of conjugated equine oestrogen , the meta-analysis found no difference in risk of breast cancer after a mean duration of 7.2 years. The observed relative risk for the combined conjugated equine oestrogen with medroxyprogesterone therapy after a mean duration of 5.6 years was similar to our findings for recent exposure, with an average duration of 3.7 years .
Don’t Miss: How To Treat Hormonal Cystic Acne
Strengths And Weaknesses Of This Study
Some limitations of this study arise from inevitable shortfalls in completeness and accuracy within any routinely collected dataset. A small proportion of women had missing information on smoking status, alcohol consumption, and BMI, but these were dealt with by multiple imputation. As we did not have reliable data for age at onset of menopause for all women, we estimated onset from the first menopause specific record before the earliest HRT prescription. For women with no such record we assumed onset within the most common age range of 50 to 54 years. We did not investigate the differences between continuous and sequential HRT because these regimens are prescribed at different times after menopause. As our cases and controls were matched by age, they would likely have been prescribed similar regimens, making a comparison infeasible. Our primary focus, anyway, was recent long term exposure.
Treatments For Vaginal Dryness
Vaginal dryness and discomfort can be bothersome menopausal symptoms for some women.
Devices that use lasers or other forms of energy to ‘rejuvenate’ vaginal tissue are now being studied as well, although it’s not yet clear how helpful they might be. It’s important to discuss the possible risks and benefits of these treatments with your doctor before deciding if one is right for you.
Read Also: Is Melatonin Good To Help You Sleep
Hormone Replacement Therapy After Breast Cancer
Many women in the UK take hormone replacement therapy to reduce menopausal symptoms. But doctors don’t routinely recommend taking HRT after breast cancer.
The concern is that HRT could increase the risk of your breast cancer coming back . The risk for women who have had breast cancer is uncertain because research so far has not drawn any firm conclusions. This might depend on the type of HRT and how long you have it.
The risk is thought to be greater in women:
- whose breast cancer has receptors for the female hormones – hormone receptor positive breast cancer
- who take HRT that contains oestrogen and progestogen
Its important that you talk to a health professional if you are finding menopausal symptoms difficult to cope with. Ideally you should speak to your cancer doctor as well as a doctor that specialises in the menopause.
Your doctor might suggest that you try other things first, such as non hormonal medicines. But they may offer HRT if your symptoms are severe. For example, if hot flushes or low mood, or a combination of symptoms are affecting your quality of life. Your doctor should discuss the risks and benefits of HRT with you.
How Does Hormone Therapy Work
About 2 out of 3 breast cancers are hormone receptor-positive. Their cells have receptors for estrogen and/or progesterone which help the cancer cells grow and spread.
There are several types of hormone therapy for breast cancer. Most types of hormone therapy either lower estrogen levels in the body or stop estrogen from helping breast cancer cells grow.
Read Also: Hormone Therapy What Is It
Hormone Replacement Therapy After Breast Cancer: Yes No Or Maybe
Breast cancer treatment including estrogen depleting therapy and chemotherapy leads to premature menopause.
-
Many breast cancer survivors suffer from intense and premature menopausal symptoms.
-
Hormone replacement therapy is avoided in this group due to concerns of increased breast cancer recurrence.
-
Evidence is not conclusive to demonstrate increased breast cancer recurrence with hormone replacement.
Patient Characteristics And History Of Mht Use
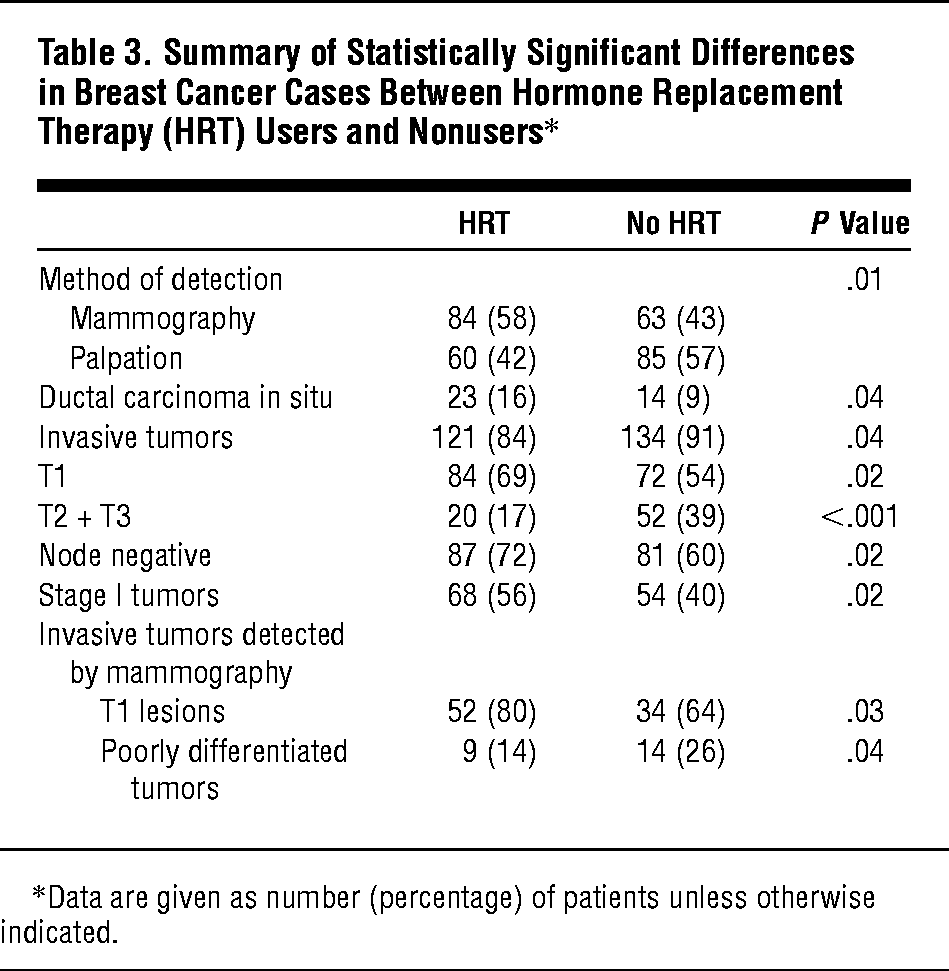
A total of 814 patients were analyzed in this study. Of the 814 patients, 433 had a history of MHT use or were current users at the time of inclusion while 381 patients had never used MHT prior to inclusion . In the group of ever MHT users, 265 had used MHT for 5 years or longer while 159 reported fewer than 5 years of use. There were significant differences in patient characteristics depending on MHT status. Ever MHT users had a lower BMI and a higher ever use of oral contraceptives vs. never MHT users. Furthermore, ever MHT users were less likely to be alcohol abstainers than never MHT users .
Table 1. History of MHT use in relation to patient and tumor characteristics.
Also Check: Side Effects Of Hormone Therapy Shots For Prostate Cancer
What Are Hormones And Hormone Receptors
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and in men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive breast cancers. Hormone-sensitive breast cancer cells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
Breast cancers that lack ERs are called ER negative, and if they lack both ER and PR they may be called HR negative.
Approximately 67%80% of breast cancers in women are ER positive . Approximately 90% of breast cancers in men are ER positive and approximately 80% are PR positive .
Types Of Studies Of Hormone Therapy And Cancer Risk
Different types of studies can be used to look at cancer risk from menopausal hormone therapy .
Randomized controlled trials: In this kind of study, a group of patients get the drug being studied , and another group gets a placebo . Results from this kind of study are powerful because which group a patient is in is based on chance. This helps assure that the groups are similar in all ways, such as risk for cancer, except for the drug thats being studied. This is the best way to see the effects of a drug. These types of studies can also be double-blinded, which means neither the people in the study nor their doctors know which group they are in. This lowers the chance that thoughts or opinions about treatment could affect the study results. Unfortunately, these kinds of studies are costly, which limits the number of people in the study, how long the study can continue, and the number of studies done.
A major drawback of observational studies is that the people getting the treatment being studied may have different cancer risk factors than the people who arent. Plus, the treatment can differ between the people being studied. This makes it less clear that the differences seen are only due to the drug being studied and not other factors.
When observational studies and randomized controlled trials have different results, most experts give more weight to the results of the randomized controlled trial.
Don’t Miss: Pills For Hormonal Imbalance Acne
Diet And Dietary Supplements
Some women find that changing the way they eat, such as eating smaller meals and avoiding triggers is helpful for them.
The effects of specific foods and dietary supplements on menopausal symptoms are not clear. This doesnt mean they wont help, but its important to understand that the evidence supporting their use is limited.
Phytoestrogens: These are estrogen-like substances found in certain plants, such as soy, red clover, and black cohosh. Some women take supplements containing these substances to try to help with symptoms of menopause.
Eating soy foods seems to be safe for breast cancer survivors, although its not clear if it can help relieve menopause symptoms. Women can get higher doses of phytoestrogens in some dietary supplements . However, not enough is known about these supplements to know for sure if they are safe and if they work. If you are considering taking one of these supplements, be sure to talk with your doctor first.
How Is Hormone Therapy Used To Treat Breast Cancer
There are three main ways that hormone therapy is used to treat hormone-sensitive breast cancer:
Adjuvant therapy for early-stage breast cancer:Tamoxifen is FDA approved for adjuvant hormone treatment of premenopausal and postmenopausal women with ER-positive early-stage breast cancer, and the aromatase inhibitorsanastrozole, letrozole, and exemestane are approved for this use in postmenopausal women.
Research has shown that women who receive at least 5 years of adjuvant therapy with tamoxifen after having surgery for early-stage ER-positive breast cancer have reduced risks of breast cancer recurrence, including a new breast cancer in the other breast, and reduced risk of death at 15 years .
Until recently, most women who received adjuvant hormone therapy to reduce the chance of a breast cancer recurrence took tamoxifen every day for 5 years. However, with the introduction of newer hormone therapies , some of which have been compared with tamoxifen in clinical trials, additional approaches to hormone therapy have become common .
Some premenopausal women with early-stage ER-positive breast cancer may have ovarian suppression plus an aromatase inhibitor, which was found to have higher rates of freedom from recurrence than ovarian suppression plus tamoxifen or tamoxifen alone .
Men with early-stage ER-positive breast cancer who receive adjuvant therapy are usually treated first with tamoxifen. Those treated with an aromatase inhibitor usually also take a GnRH agonist.
Read Also: Is Male Hormone Replacement Therapy Safe
Menopausal Hormone Therapy And Cancer Risk
For decades, women have used hormone therapy to ease symptoms of menopause, such as hot flashes and sweating. This is called menopausal hormone therapy, and you may see it abbreviated as HT or MHT. You may also hear it described as hormone replacement therapy , postmenopausal hormone therapy , or postmenopausal hormones .
In the past, many doctors and their patients believed that MHT didnt just help with hot flashes and other symptoms it had important health benefits. But well-conducted studies have led many doctors to conclude that the risks of MHT often outweigh the benefits.
This information covers only how MHT can affect a womans risk of getting certain cancers. It does not cover other possible risks of MHT such as heart disease or stroke.
You can use this information when you talk to your doctor about whether MHT is right for you.
Can I Take Menopausal Hormone Therapy After Breast Cancer
When women reach menopause, some choose to take PHT, which is made up of female hormones to help reduce menopause symptoms. But there have been concerns about women who have had breast cancer using PHT, because of the known link between estrogen levels and breast cancer growth.
A well-designed clinical trial found that breast cancer survivors taking PHT were much more likely to develop a new or recurrent breast cancer than women who were not taking these hormones. Because of this, doctors generally do not recommend PHT if a woman was previously treated for breast cancer.
Don’t Miss: Can I Give My Child Melatonin Every Night