Orteronel Misses Goal In Metastatic Hormone
Significant improvement seen in progression-free survival, but not overall survival, with addition of orteronel to androgen deprivation therapy
- HealthDay
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
What Are The Side Effects Of Hormone Therapy For Prostate Cancer
Because androgens affect many other organs besides the prostate, ADT can have a wide range of side effects , including:
- loss of interest in sex
Studer UE, Whelan P, Albrecht W, et al. Immediate or deferred androgen deprivation for patients with prostate cancer not suitable for local treatment with curative intent: European Organisation for Research and Treatment of Cancer Trial 30891. Journal of Clinical Oncology 2006 24:18681876.
Zelefsky MJ, Eastham JA, Sartor AO. Castration-Resistant Prostate Cancer. In: Vincent T. DeVita J, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology, 9e. Philadelphia, PA: Lippincott Williams & Wilkins 2011.
Smith MR, Saad F, Chowdhury S, et al. Apalutamide and overall survival in prostate cancer. European Urology 2021 79:150158.
Key Factors Associated With Adt Alone Use: Adt Alone Vs Chemotherapy Or Nha
Examining the key clinical reasons for treatment choice revealed that physicians prescribed ADT alone vs chemotherapy to significantly higher proportions of patients with a poor performance status , who wanted to maintain/improve their QoL , who may have compliance challenges , who could not tolerate adverse events , or with bone only disease . The only significant difference between ADT alone vs NHA in terms of key clinical reasons for treatment choice was for treatment is suitable for patients who may have compliance challenges, with physicians prescribing ADT alone rather than NHA to a significantly higher proportion of patients . All key clinical reasons for treatment choice for ADT alone vs NHA or chemotherapy are presented in Fig. .
Don’t Miss: Hormone Replacement Therapy Augusta Ga
Treatment Of The Primary Tumour
The last decade has seen much debate amongst prostate cancer specialists in regard to cytoreductive treatment for the primary tumour. Two large trials have revealed answers pertaining to external beam radiotherapy in this space, however, the specific cohorts of patients that would benefit from ERBT and the field of ERBT used should be further refined. Furthermore, studies comparing cytoreductive prostatectomy to standard treatment need to be carried out.
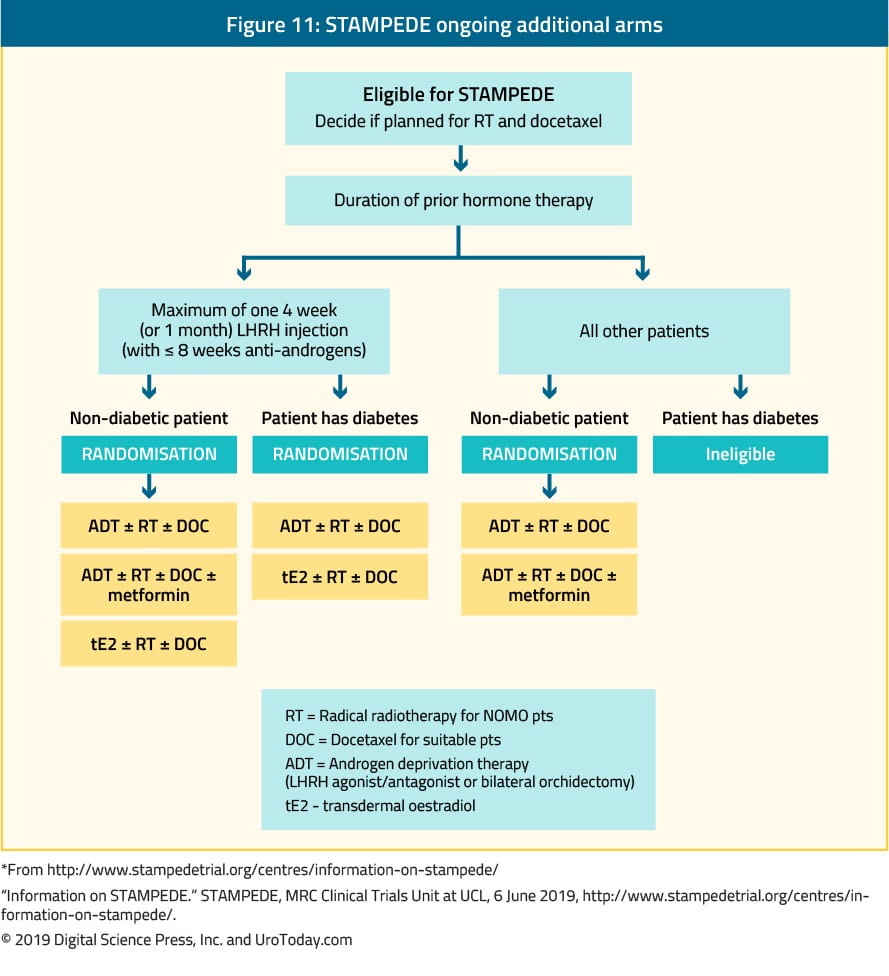
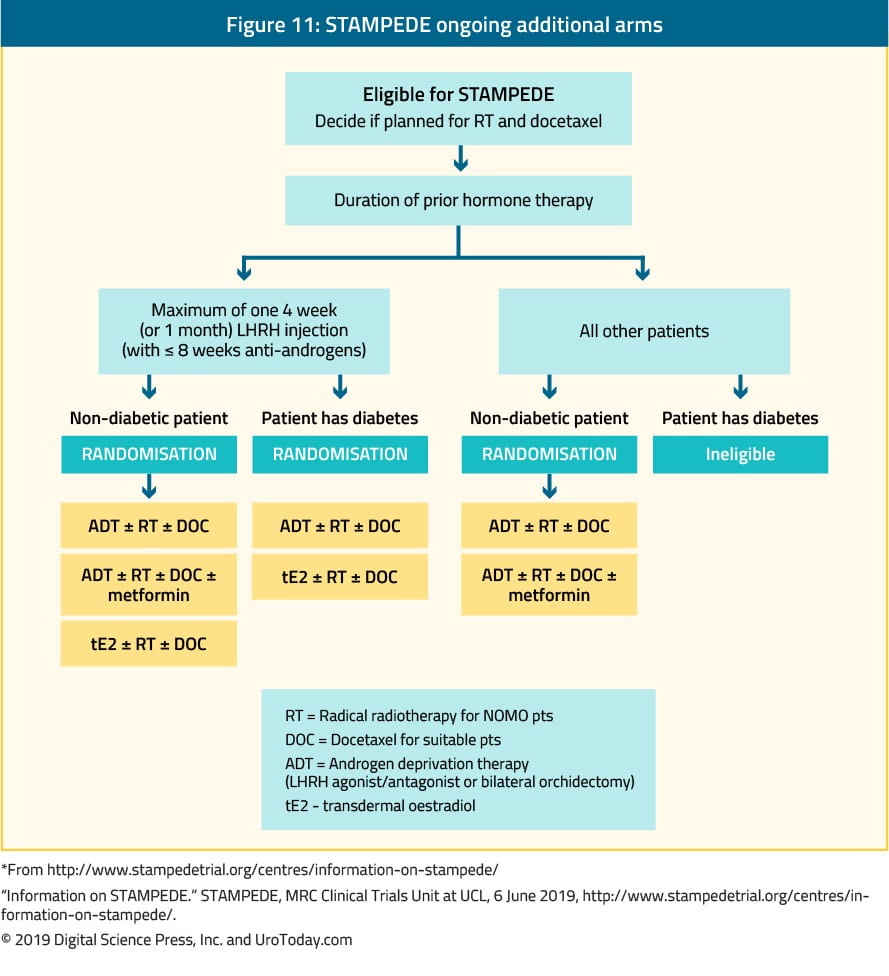
The evidence for ERBT to the primary tumour is primarily derived from the STAMPEDE trial and HORRAD trial with results from the PEACE-1 trial eagerly awaited. The HORRAD trial recruited 432 men with PSA > 20 ng/mL and primary bone metastases on whole body bone scan. These men were randomised to receive ADT with or without ERBT . With median follow up of 47 months, improvement in OS was not shown with added ERBT. However in a subgroup analysis of patients with low metastatic burden , radiotherapy resulted in a non-significant improvement in OS . The STAMPEDE trial randomised 2061 men with newly diagnosed mHSPC to receive standard therapy with or without ERBT . Around 60% of these men had high metastatic burden. Results showed that for all patients, failure free survival was improved but not OS. However, failure free survival and OS were both improved specifically for patients with low metastatic burden .
Patient Demographics And Clinical Characteristics
Patient demographics and clinical characteristics are presented in Table . Pairwise analyses revealed several significant differences between treatment groups , including for most recent PSA level, risk status and disease volume . Men treated with NHA or chemotherapy vs ADT alone had significantly higher PSA levels . Similarly, significantly higher proportions of patients receiving NHAs or chemotherapy vs ADT alone had high-risk status and high disease volume .
Table 3 Patient demographics and clinical characteristics
Recommended Reading: Where Do You Get Your Hormones Tested
Current Treatment Options For Newly Diagnosed Metastatic Hormone
Sean Ong1,2^, Jonathan OBrien1,3, Elizabeth Medhurst1, Nathan Lawrentschuk1,2,3, Declan Murphy1,4, Arun Azad4,5
1 EJ Whitten Foundation Prostate Cancer Research Centre, Epworth Health , Sir Peter MacCallum Department of Oncology , , Australia
Contributions: Conception and design: D Murphy, A Azad Administrative support: None Provision of study materials or patients: None Collection and assembly of data: All authors Data analysis and interpretation: None Manuscript writing: All authors Final approval of manuscript: All authors.
^ORCID: 0000-0003-1117-2409.
Correspondence to:
Keywords: Prostate cancer metastatic hormone-sensitive management
Submitted Jul 29, 2020. Accepted for publication Jan 05, 2021.
doi: 10.21037/tau-20-1118
Early Versus Delayed Treatment
For men who need hormone therapy, such as men whose PSA levels are rising after surgery or radiation or men with advanced prostate cancer who dont yet have symptoms, its not always clear when it is best to start hormone treatment. Some doctors think that hormone therapy works better if its started as soon as possible, even if a man feels well and is not having any symptoms. Some studies have shown that hormone treatment may slow the disease down and perhaps even help men live longer.
But not all doctors agree with this approach. Some are waiting for more evidence of benefit. They feel that because of the side effects of hormone therapy and the chance that the cancer could become resistant to therapy sooner, treatment shouldnt be started until a man has symptoms from the cancer. This issue is being studied.
Don’t Miss: How To Get Rid Of Hormonal Weight
Hormone Therapy For Prostate Cancer
Jump to a section
Hormone therapy is also called androgen suppression therapy. The goal of this treatment is to reduce levels of male hormones, called androgens, in the body, or to stop them from fueling prostate cancer cell growth.
Androgens stimulate prostate cancer cells to grow. The main androgens in the body are testosterone and dihydrotestosterone . Most androgens are made by the testicles, but the adrenal glands as well as the prostate cancer cells themselves, can also make androgens.
Lowering androgen levels or stopping them from getting into prostate cancer cells often makes prostate cancers shrink or grow more slowly for a time. But hormone therapy alone does not cure prostate cancer.
Possible Future Treatment Strategy As Per The Clinical And Biological Characteristics
The treatment strategies should be determined as per cancer and patient characteristics as well as patient preference. We showed the possible treatment strategy for patients with mCSPC as per patient subgroups . Group 1: elderly and/or fragile patients with very limited life expectancy ADT alone or best supportive care. Group 2-a: patients with low-volume, low-risk disease, favorable response to ADT, and life expectancy < 10 y ADT alone, because long-term OS, about 10 years, is expected with ADT alone in this patient group. Adverse events caused by upfront combination therapies may exceed their efficacy in those patients. Group 2-b: patients with the same cancer characteristics as group 2-a patients and having longer life expectancy upfront combination therapies using docetaxel or ARPIs, with or without prostatectomy or EBRT to the prostate together with ADT. Metastases-directed radiotherapy may be also indicated. Complete eradication of cancer and cure may be anticipated with these aggressive combination treatments in these patients. Group 3: patients with high-volume, high-risk, or unfavorable response to ADT upfront combination therapies using docetaxel or ARPIs. Group 4: patients carrying DDR gene mutations poly polymerase inhibitors or platinum-based chemotherapy. The prognostic and predictive biomarker-based decision will enable optimal personalized treatment.
Also Check: How To Increase Melatonin Naturally
Justification For A New Guideline
Clinicians treating men with advanced prostate cancer are challenged with the rapidly evolving prostate cancer landscape given the approval of new classes of agents for use in various prostate cancer disease states. The increasing complexity of advanced prostate cancer management underscores the need for the current clinical practice guideline, developed to provide a rational basis for treatment of patients with advanced disease, based on currently available published data. To assist in clinical decision-making, guideline recommendations are furnished according to disease state across the entire continuum of advanced prostate cancer.
Combined With Adt The Androgen
byMike Bassett, Staff Writer, MedPage Today September 7, 2022
In combination with androgen deprivation therapy , the novel androgen-receptor inhibitor rezvilutamide significantly improved radiographic progression-free survival and overall survival compared with bicalutamide in patients with high-volume, metastatic, hormone-sensitive prostate cancer, the phase III CHART trial showed.
Among 654 mostly Asian patients, median radiographic PFS was not reached in the rezvilutamide group compared with 25.1 months in the bicalutamide group at a median follow-up of 21.2 months, and overall survival was not reached in either group at a median follow-up of 29.3 months, reported Dingwei Ye, MD, of Fudan University Shanghai Cancer Center in China, and colleagues.
The 2-year radiographic PFS rate was 72.3% in the rezvilutamide group and 50.0% in the bicalutamide group, while the 2-year OS rates were 81.6% and 70.3%, respectively, they noted in Lancet Oncology.
The benefits of rezvilutamide on radiographic PFS were observed in all subgroups, except for patients with visceral metastases and those not from China.
Rezvilutamide will be a welcome addition to the range of androgen-receptor inhibitors already available, and will we hope through a little healthy competition, overcome some of the barriers to real-world use of doublet therapy, such as cost and access, Kostos and Murphy wrote.
Disclosures
The study was funded by Jiangsu Hengrui Pharmaceuticals.
Primary Source
Read Also: Where Can I Buy Liquid Melatonin
Treatment To Lower Androgen Levels From Other Parts Of The Body
LHRH agonists and antagonists can stop the testicles from making androgens, but cells in other parts of the body, such as the adrenal glands, and prostate cancer cells themselves, can still make male hormones, which can fuel cancer growth. Some drugs can block the formation of androgens made by these cells.
Abiraterone blocks an enzyme called CYP17, which helps stop these cells from making androgens.
Abiraterone can be used in men with advanced prostate cancer that is either:
- Castration-resistant
This drug is taken as pills every day. It doesnt stop the testicles from making testosterone, so men who havent had an orchiectomy need to continue treatment with an LHRH agonist or antagonist. Because abiraterone also lowers the level of some other hormones in the body, prednisone needs to be taken during treatment as well to avoid certain side effects.
Ketoconazole , first used for treating fungal infections, also blocks production of androgens made in the adrenal glands, much like abiraterone. It’s most often used to treat men just diagnosed with advanced prostate cancer who have a lot of cancer in the body, as it offers a quick way to lower testosterone levels. It can also be tried if other forms of hormone therapy are no longer working.
Ketoconazole also can block the production of cortisol, an important steroid hormone in the body, so men treated with this drug often need to take a corticosteroid .
From Personalized To All
A systematic review and meta-analyses of the aggregate data of the CHAARTED, GETUG-AFU15, and STAMPEDE trials indicated that the upfront use of docetaxel showed better OS in patients with mCSPC than in those with ADT alone . As per the STAMPEDE trial, upfront docetaxel improved the OS irrespective of the metastatic tumor burden . For low-volume patients, the median OS was 93.2 mon and 76.7 mon for upfront docetaxel and ADT alone, respectively . This HR was consistent with that in high-volume patients , suggesting that upfront docetaxel would be beneficial for all patients with mCSPC, irrespective of the metastatic burden, and this treatment may be for all-comers.
These recent clinical trials suggest that early combination therapies are consistently associated with better outcomes than ADT alone, irrespective of the tumor burden and risk category. Thus, recent clinical guidelines recommend a combination of docetaxel or ARPIs with ADT as first-line therapy for all patients with mCSPC., The era of ADT alone may end and upfront combination therapies are becoming a standard of care as the initial treatment for all-comers with mCSPC.
Also Check: How To Dose Melatonin For Sleep
The Role Of The Urologist
Management of mHSPC has traditionally been in the domain of the urologist. Since ADT was standardised as a first-line option for these patients many years ago, it has been the urologist who has been the primary specialist overseeing their care until the emergence of castration-resistance. However, the upfront use of Docetaxel chemotherapy and ARPIs has led to changes in patterns of care, with medical oncologists playing an increasing role in the primary management of mHSPC. Whilst Docetaxel is most often administered by medical oncologists, it is also administered by urologists in some countries, especially in the Asia-Pacific region . The increasing role for well tolerated oral ARPIs combined with ADT for mHSPC, also means that urologists can continue to play a key role in the management of mHSPC, provided they are willing to become facile with the safe use and monitoring of these agents . Ultimately, these patients are best managed in multidisciplinary teams, taking into account patient and disease factors, as well as access and affordability issues .
Improving How Long Patients Live
The ENZAMET trialfunded in part by the drugs manufacturer, Astellas Pharma, as well as government health agencies in Canada and Australiaenrolled more than 1,100 men with hormone-sensitive metastatic prostate cancer. The men were randomly assigned to ADT combined with enzalutamide or with any of three other androgen-blocking drugs.
At a median follow-up of nearly 3 years, men who received ADT plus enzalutamide had a 33% reduced risk of death, with 80% still alive compared with 72% of men treated with ADT plus another antiandrogen drug, reported the trials lead investigator, Christopher Sweeney, M.B.B.S., of the Dana-Farber Cancer Institute.
Men in the enzalutamide group also had better clinical progression-free survival , which the research team defined as the time until the return of disease-related symptoms, the detection of new metastases on imaging scans, or the initiation of another cancer treatment for prostate cancer, whichever came first. At 3 years, 63% of men in the enzalutamide group were alive without clinical progression of their disease, compared with 33% in the standard treatment group.
Although enzalutamide appeared to be effective regardless of whether men had high- or low-volume disease, one apparent differentiating factor was planned early treatment with docetaxel. Nearly half of the men in both treatment groups received early treatment with docetaxel and, for those men, enzalutamide was not associated with longer overall survival.
Read Also: Will Testosterone Pills Help Build Muscle
Definitive Treatment Is Beneficial Only In Patients With Low
Not only systemic pharmacotherapy, but radiation to the prostate also improves OS in low-volume disease. The recent high-quality RCTs, STAMPEDE and Hormonal Therapy Versus Hormonal Therapy Plus Local External Radiation Therapy in Patients With Primary Diagnosed Metastasized Prostate Cancer , concluded that adding radiation therapy to the prostate in mCSPC patients receiving ADT did not further improve their OS, the primary endpoint. In contrast, subgroup analyses by metastatic burden in the STAMPEDE trial showed OS benefit for patients with low-volume disease . The HORRAD trial also showed a similar trend without statistical significance in patients with < 5 metastatic lesions. Meta-analysis of 2 RCTs that involved 2493 patients suggested that ADT plus EBRT to the prostate was associated with improved OS as compared to ADT alone in men with low-volume metastatic burden however, this result was not observed in those with high-volume disease . Prostatectomy may also improve the oncologic outcomes in patients with oligometastatic prostate cancer. The definitive treatments, either radiation or prostatectomy, may be associated with survival benefit in patients with low metastatic burden. The results of several ongoing clinical trials on the benefit of prostatectomy and radiation to the prostate are expected to provide more information on this subject.
Relevance Of Trial Data In Real
After decades without significant progress in the treatment landscape of mHSPC, the results of the above-mentioned trials are welcome. Nevertheless, we need to cautiously interpret these results, taking into consideration the between-study heterogeneity in study populations, and how well they reflect our patient population .
Recommended Reading: How Do You Balance Hormones Naturally
How Does Hormone Therapy Work Against Prostate Cancer
Early in their development, prostate cancers need androgens to grow. Hormone therapies, which are treatments that decrease androgen levels or block androgen action, can inhibit the growth of such prostate cancers, which are therefore called castration sensitive, androgen dependent, or androgen sensitive.
Most prostate cancers eventually stop responding to hormone therapy and become castration resistant. That is, they continue to grow even when androgen levels in the body are extremely low or undetectable. In the past, these tumors were also called hormone resistant, androgen independent, or hormone refractory however, these terms are rarely used now because the tumors are not truly independent of androgens for their growth. In fact, some newer hormone therapies have become available that can be used to treat tumors that have become castration resistant.
Searches And Article Selection
A research librarian conducted searches in Ovid MEDLINE , Cochrane Central Register of Controlled Trials , and Cochrane Database of Systematic Reviews . An updated search was conducted prior to publication through January 20, 2020. The methodology team supplemented searches of electronic databases with the studies included in the prior AUA review and by reviewing reference lists of relevant articles.
The methodology team developed criteria for inclusion and exclusion of studies based on the Key Questions and the populations, interventions, comparators, outcomes, and settings of interest. The population was patients with advanced prostate cancer as described in Table 3. Treatments included first and second line antiandrogens, immunotherapy, chemotherapy, radiation therapy, surgery, radiopharmaceuticals, and surveillance strategies. Comparisons were against placebo, no therapy, or another active intervention and intermittent versus continuous therapy. Outcomes included overall survival , prostate cancer mortality, progression-free survival , prostate-specific antigen progression-free survival , failure-free survival, metastases-free survival, time to metastases, time to progression, skeletal events, and adverse events.
Don’t Miss: What Birth Control Does Not Have Estrogen