Why It Is Important To Do This Review
Survival of patients with endometrial cancer has not improved substantially over the past 25 years and although most cases are detected and treated in early stages, a significant number of women present at advanced stage . Often these patients suffer from major co-morbidities and consequently, aggressive chemotherapy and/or surgery may not be beneficial or may even be harmful.
Phase II studies have demonstrated a high response rate in some of the hormonal agents and considering their favourable toxicity profile, they could be extremely useful for patients with advanced or recurrent endometrial cancer. Kauppila et al completed a review of progestin therapy of endometrial, breast and ovarian carcinoma . However, it was not a systematic review and details of the type of studies included were not stated. Also, it was carried out more than 20 years ago and additional experience from studies that followed could lead to new recommendations regarding hormonal treatment in advanced or recurrent endometrial cancer.
Data Extraction And Quality Assessment
Data from included articles was extracted using data collection forms with information regarding study design, in- and exclusion criteria, number of included patients, age, tumor stage and grade, estrogen and progesterone receptor status, previous treatment and complete response , partial response , stable disease , progressive disease, progression free survival , and overall survival was noted. Additional information was requested from study authors if necessary.
The quality of each individual study was assessed in five domains based of the National Institute of Health Quality Assessment Tool for Case Series Studies . Each full-text article was evaluated independently by three authors and risk of bias was subsequently discussed in a consensus meeting.
Importance Of Patient Selection
A question that clinicians must answer before considering a patient as a candidate for hormonal therapy is whether the recurrent tumor still expresses the hormone receptors needed for successful treatment. There are precedents in the literature indicating that progression of endometrial cancer is associated with loss of hormone receptors. For example, investigators at Memorial Sloan Kettering Cancer Center examined 34 cases of endometrial cancer in which primary and recurrent tumors were available.30 In addition to histologic classification, primary and matched recurrent tumors were analyzed for expression of PR as well as other markers of interest, such as p53, p16, and DNA mismatch repair proteins . Compared with endometrioid carcinoma patients, serous carcinoma patients were older, presented at a higher stage, and had shorter survival. Serous carcinomas were the most common recurrent endometrial carcinoma, and 62% displayed similar morphology when comparing primary and recurrent carcinomas. Seven of 13 endometrioid carcinomas had morphologically discordant recurrence. Serous and morphologically ambiguous carcinomas demonstrated relative morphologic fidelity compared with endometrioid carcinomas.
You May Like: What Is The Best Vitamins To Take For Hormonal Imbalance
The Extrinsic Death Receptor Pathway
The extrinsic pathway is activated by members of two protein families, the tumor necrosis factor family and the receptors for these ligands . For example, FasL binds to Fas TNF binds to TNFRI Apo3 ligand binds to DR3 and TRAIL binds to DR4 and DR5 . The salient point of death receptor signaling is the formation of the death inducing signaling complex . Upon activation of death receptors, such as Fas, the cytoplasmic adaptor molecule Fas-associated death domain interacts with the intracellular regions of the receptor proteins. The apoptotic signal is then transduced to pro-caspase-8 upon the interaction of FADD with pro-caspase-8 . The pro-domain of caspase-8 remains at the DISC, while active caspase-8 dissociates from the DISC, which is further released into the cytosol to propagate the apoptotic signal by initiating intracellular members of caspase family, mainly caspase-3. Several inhibitory proteins for this pathway have been characterized, like FADD-like interleukin-1 converting enzyme/caspase-8 inhibitory protein , Fas associated phospahatase-1 , and soluble Fas . Overexpression of any of these molecules can lead to resistance to Fas mediated apoptosis in endometrial cancer .
Immunotherapy And Targeted Therapy

Immunotherapy is a type of cancer treatment that helps your immune system fight cancer, according to National Cancer Institute . Targeted therapy, per the NCI, is “a type of cancer treatment that targets proteins that control how cancer cells grow, divide, and spread.”
In July 2021, the US Food and Drug Administration approved a combination of Keytruda , which is an immunotherapy, and Lenvima , a targeted therapy, as a treatment for patients with certain types of advanced endometrial cancers.
Both pembrolizumab and lenvatinib independently work in a small percentage of patients with endometrial cancer, but when given together, they produce a “synergistic” effect, explains Dr. Schram. For patients whose cancer has metastasized or whose cancer has come back, the combination of these two therapies plus chemo is typically given as first-line treatment, says Dr. Schram.
Other targeted therapies, such as trastuzumab and bevacizumab, are sometimes used to treat certain types of uterine cancer as well, the American Society of Clinical Oncology points out.
Don’t Miss: Is Male Hormone Replacement Therapy Safe
The Intrinsic Mitochondrial Pathway
The intrinsic pathway is usually activated in response to intracellular stress signals and extracellular apoptotic stimuli . The intrinsic apoptotic pathway is dominated by the Bcl-2 family of proteins, which regulate the release of cytochrome c from the mitochondria . Following a death signal, the pro-apoptotic Bax and Bak undergo a conformational change resulting in their integration into the mitochondrial outer membrane where it appears that they antagonize the function of pro-survival Bcl-2 proteins . Bax homodimers and heterodimers then interact with a voltage-dependent anion channel in the mitochondrial outer membrane to release cytochrome c by increasing mitochondrial membrane permeability via opening of the mitochondrial permeability transition pore . The release of cytochrome c results in the formation of an apoptosome complex , which consists of apoptosis activating factor-1 and procaspase-9 in the presence of dATP/ATP. Procaspase-9 promotes its self-activation . The activated initiator caspase i.e. caspase-9, leads to activation of one of the effector caspases, which can be caspase-3, -6 or -7. The active caspase further cleaves an inhibitor of caspase-activated DNase lamins, several cytoskeleton binding proteins and poly polymerase . Cleavage of these proteins causes DNA fragmentation, inhibition of DNA synthesis and repair, nuclear membrane disruption, chromatin condensation, and cytoskeleton collapse.
Surgery To Stop The Ovaries From Working
This is also a type of ovarian ablation. You might choose to have an operation to remove your ovaries instead of having drug treatment to stop them working. You have this operation as keyhole surgery. It is called laparoscopic oophorectomy and you have it under general anaesthetic . You usually stay in hospital overnight.
The surgeon makes a number of small cuts into your tummy . They put a long bendy tube called a laparoscope into one of the cuts. The laparoscope connects to a video screen.
The surgeon puts small instruments through the other cuts to carry out the operation and remove the ovaries. They close the cuts with stitches and cover them with small dressings.
Removing your ovaries causes you to have a sudden menopause. The symptoms include hot flushes, sweating and mood swings.
Dont Miss: Food That Help With Hormonal Imbalance
Recommended Reading: How Long Is Hormone Therapy For Prostate Cancer
Hormone Therapy For Breast Cancer Treatment
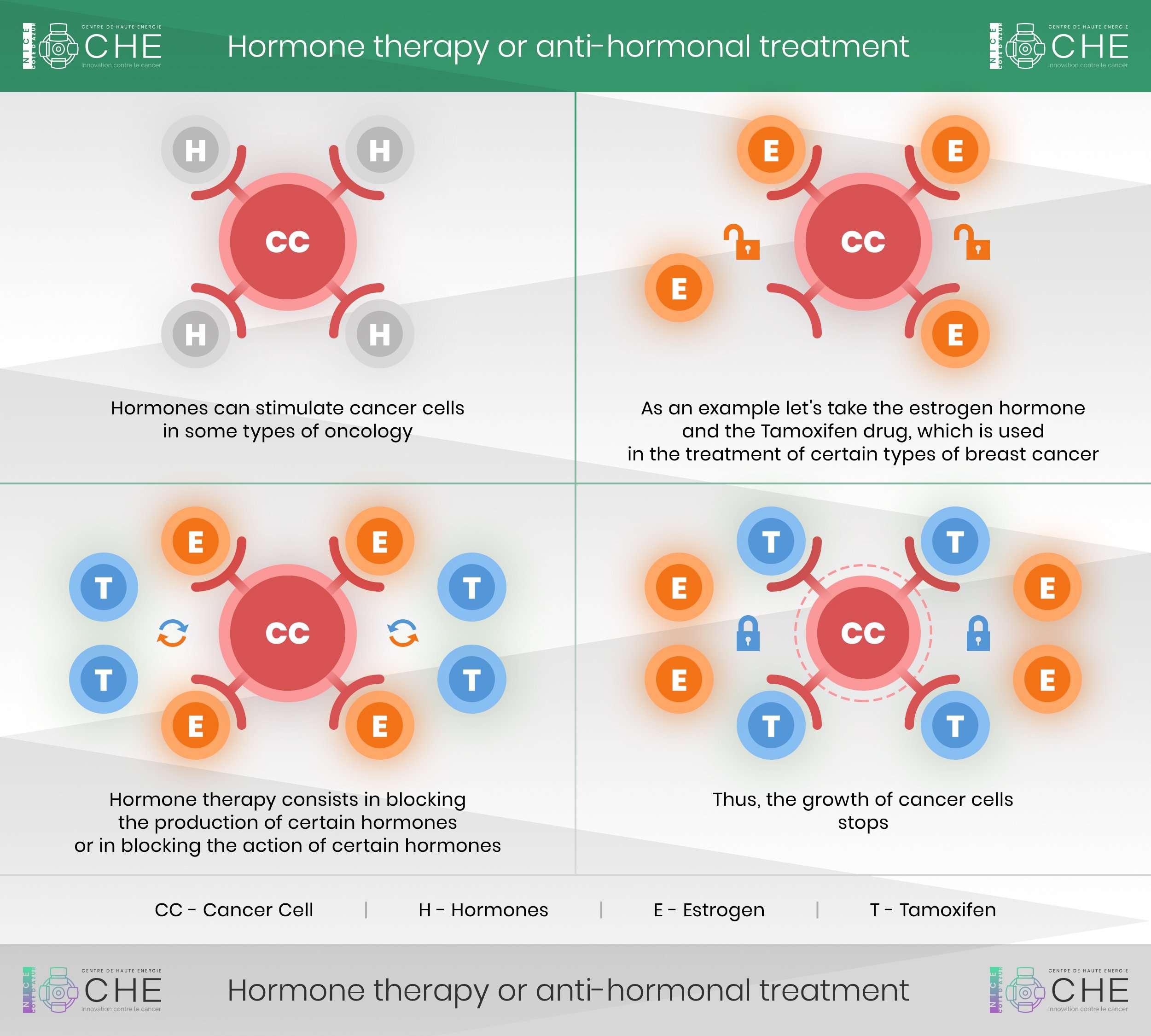
Most cases of breast cancer are fueled by the hormones estrogen and progesterone. Hormone therapy, also called endocrine therapy, is used to remove or block hormones and stop or slow down the growth of cancer cells. If your cancer is hormone-sensitive, then hormone therapy may be part of your treatment plan.
If your healthcare professional prescribes this for your early-stage breast cancer, plan on taking hormonal therapy for five years after completing your primary treatments. The main benefit of this type of therapy is to prevent estrogen from fueling estrogen-responsive positive cancer cells, thus reducing your risk of recurrence. For breast cancer that is estrogen receptor-negative, hormonal therapy is not effective.
Dont Miss: How Do You Check Your Testosterone Level
Whats The Survival Rate For People With Uterine Cancer
The five-year survival rate for endometrial cancer is 81%. That means 81% of people diagnosed with the disease are alive five years later. The rate is even higher when cancer is localized and hasnt spread outside the uterus. Then the survival rate reaches as high as 95%. Treatments continue to improve, along with survival rates.
You May Like: Hormone Issue That Prevents Ovulation
Hormone Therapy For Uterine Sarcomas
Hormone therapy is the use of hormones or hormone-blocking drugs to treat cancer. Part of diagnosing uterine sarcoma includes tests that check the cancer cells to see if they have receptors where hormones can attach. If they do have these receptors , hormone treatment might be a good option. Hormone therapy is mainly used to treat low-grade endometrial stromal sarcomas and is rarely used for the other types of uterine sarcomas.
For The Population Studied As A Whole There Was An Overall Deterioration In The Quality Of Life At Two Years From Diagnosis This Deterioration Was Greater In Patients Who Had Received Hormone Therapy Especially After The Menopause By Contrast Chemotherapy Had A Bigger Effect On Quality Of Life In Non
It is important in the future that we are able to predict which women are going to develop severe symptoms with anti-hormonal treatment so that we can support them, added Dr Vaz-Luis. While it has been shown that hormone therapy provides a real benefit in reducing the relapse rate of hormone-dependent cancers which represent 75% of all breast cancers, the deterioration in quality of life may also have a negative effect on patient adherence to treatment. It is, therefore, important to offer them symptomatic treatment, in particular for menopausal symptoms, musculoskeletal pain, depression, severe fatigue and cognitive dysfunction and to combine this with supportive measures such as physical exercise and cognitive behaviour therapy.
Also Check: What Does Estrogen Do For You
Read Also: What Mg Of Melatonin Should I Take
Outcome Assessment And Statistical Analyses
The primary outcome was the response rate to hormonal therapy and was defined as the proportion of patients with CR and PR. Other outcomes were the clinical benefit rate , which is defined as the proportion of patients with either CR, PR, or SD and toxicity which is defined as any adverse event occurring during treatment. Toxicity was ideally evaluated with a standardized measuring scale including grading of severity. Individual treatment arms of randomized studies were analyzed separately. RR and CBR are reported for tamoxifen, other SERMs/SERDs, aromatase inhibitors, combination regimens and for ER positive and negative tumors separately. The specific expression of the two ER isoforms was not considered. Due to the large heterogeneity in the included studies, meta-analysis could not be performed. In case it was not reported in the study, the 95% confidence interval for RR and CBR was calculated using the normal approximation method of the binomial confidence interval .
Results Of Direct Comparisons
The nine studies comprised 2133 patients. The duration of treatment was from 12 to 24 weeks. An investigation into the optimal duration of exemestane was reported in one study. To make a distinction, we defined exemestane if the duration of exemestane was less than 20 weeks, and exemestane if the treatment duration was than 20 weeks. There were three arms in two studies, respectively. One study was about anastrozole plus different treatment protocols of gefitinib compared with anastrozole, and we considered anastrozole versus anatrozole plus gifitinib. As a result, ten arms were assessed including, chemotherapy, tamoxifen, letrozole, anastrozole, exemestane , exemestane , anastrozole plus tamxifen, letrozole plus everomilus, anatrozole plus gefitinib, and exemestane plus celecoxib. All patients were postmenopausal women diagnosed with non-metastatic breast cancer. All patients except for four were HR-positive. Four studies reported the levels of HER2,,,. Characteristics of the eligible studies are listed in .
You May Like: How To Boost Estrogen Naturally
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning.
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place , nearby , or in another place . Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. A key goal of follow-up care is to watch for a recurrence and to manage possible late effects and long-term side effects from treatment. Learn more about coping with the fear of recurrence.
Some symptoms of recurrent cancer are similar to those experienced when the disease was first diagnosed:
-
Vaginal bleeding or discharge
-
Pain in the pelvic area, abdomen, or back of the legs
-
Difficulty or pain when urinating
-
Persistent cough/shortness of breath
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence.
Potential Biases In The Review Process
A comprehensive search was performed, including a thorough search of the grey literature and all studies were sifted and data extracted by at least two review authors independently. We restricted the included studies to RCTs as they provide the strongest level of evidence available. Hence we have attempted to reduce bias in the review process.
The greatest threat to the validity of the review is likely to be the possibility of publication bias, i.e. studies that did not find the treatment to have been effective may not have been published. We were unable to assess this possibility as all the treatment comparisons were restricted to single-trial analyses.
We included trials of women with all stages of disease and analysed the subgroups of advanced/recurrent endometrial cancer cases. There is a possibility that patient characteristics in these trials may be heterogeneous compared to trials including only patients with advanced/recurrent disease, although you would expect the randomisation process to put patients with similar baseline demographics in each group.
Also Check: Do Hormonal Iuds Cause Weight Gain
What Causes Uterine Cancer
Researchers arent sure of the exact cause of uterine cancer. Something happens to create changes in cells in your uterus. The mutated cells grow and multiply out of control, which can form a mass called a tumor.
Certain risk factors can increase the chances youll develop uterine cancer. If youre at high risk, talk to your healthcare provider about steps you can take to protect your health.
Can Hormone Therapy Be Used To Prevent Breast Cancer
Yes. Most breast cancers are ER positive, and clinical trials have tested whether hormone therapy can be used to prevent breast cancer in women who are at increased risk of developing the disease.
A large NCI-sponsored randomized clinical trial called the Breast Cancer Prevention Trial found that tamoxifen, taken for 5 years, reduces the risk of developing invasive breast cancer by about 50% in postmenopausal women who were at increased risk . Long-term follow-up of another randomized trial, the International Breast Cancer Intervention Study I, found that 5 years of tamoxifen treatment reduces the incidence of breast cancer for at least 20 years . A subsequent large randomized trial, the Study of Tamoxifen and Raloxifene, which was also sponsored by NCI, found that 5 years of raloxifene reduces breast cancer risk in such women by about 38% .
As a result of these trials, both tamoxifen and raloxifene have been approved by the FDA to reduce the risk of developing breast cancer in women at high risk of the disease. Tamoxifen is approved for this use regardless of menopausal status. Raloxifene is approved for use only in postmenopausal women.
Read Also: What Is Natural Hormone Replacement
Whos At Risk For Uterine Cancer
There are several risk factors for endometrial cancer. Many of them relate to the balance between estrogen and progesterone. These risk factors include having obesity, a condition called polycystic ovarian syndrome or taking unopposed estrogen . A genetic disorder known as Lynch syndrome is another risk factor unrelated to hormones.
Risk factors include:
Age, lifestyle and family history:
- Age: As you get older, your likelihood of developing uterine cancer increases. Most uterine cancers occur after age 50.
- Diet high in animal fat: A high-fat diet can increase your risk of several cancers, including uterine cancer. Fatty foods are also high in calories, which can lead to obesity. Extra weight is a uterine cancer risk factor.
- Family history: Some parents pass on genetic mutations for hereditary nonpolyposis colorectal cancer . This inherited condition raises the risk for a range of cancers, including endometrial cancer.
Other conditions:
- Diabetes: This disease is often related to obesity, a risk factor for cancer. But some studies suggest a more direct tie between diabetes and uterine cancer as well.
- Obesity : Some hormones get changed to estrogen by fat tissue, raising uterine cancer risk. The higher the amount of fat tissue, the greater the effect on estrogen levels.
- Ovarian diseases: People who have certain ovarian tumors have high estrogen levels and low progesterone levels. These hormone changes can increase uterine cancer risk.
Menstrual and reproductive history:
Treatments To Stop Ovarian Function In Premenopausal Women
Women who havent undergone menopause â either naturally or as a result of cancer treatment â may opt to undergo treatment to stop their ovaries from producing hormones.
Options may include:
- Surgery to remove the ovaries
- Radiation therapy aimed at the ovaries
- Medications, such as goserelin
Treatments to stop ovarian function may allow premenopausal women to take medications only available to postmenopausal women.
Also Check: Can You Take Melatonin Every Day
Also Check: Will My Doctor Prescribe Testosterone