Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer.
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Brca1 And Brca2 Genetic Mutations
Most inherited cases of breast cancer are associated with mutations in two genes: BRCA1 and BRCA2 .
Everyone has BRCA1 and BRCA2 genes. The function of the BRCA genes is to repair cell damage and keep breast, ovarian, and other cells growing normally. But when these genes contain mutations that are passed from generation to generation, the genes don’t function normally and breast, ovarian, and other cancer risk increases. BRCA1 and BRCA2 mutations may account for up to 10% of all breast cancers, or 1 out of every 10 cases.
Having a BRCA1 or BRCA2 mutation doesn’t mean you will be diagnosed with breast cancer. Researchers are learning that other mutations in pieces of chromosomes called SNPs may be linked to higher breast cancer risk in women with a BRCA1 mutation as well as women who didn’t inherit a breast cancer gene mutation.
Women who are diagnosed with breast cancer and have a BRCA1 or BRCA2 mutation often have a family history of breast cancer, ovarian cancer, and other cancers. Still, most people who develop breast cancer did not inherit a genetic mutation linked to breast cancer and have no family history of the disease.
You are substantially more likely to have a genetic mutation linked to breast cancer if:
If one family member has a genetic mutation linked to breast cancer, it does not mean that all family members will have it.
Guidelines For Elective Surgical Options
Women with BRCA1 or BRCA2 mutations face a significant risk of breast and ovarian cancer. Prophylactic removal of the fallopian tubes and ovaries is recommended by about age 40. Many women with BRCA1 or BRCA2 mutations will also elect to have their breasts removed. Nipple-sparing mastectomy is an effective option for these women.
Making the decision to have an elective preventive double mastectomy and removal of the ovaries is personal and should be based on many life factors. You must balance where you are in your childbearing years, what your future choices may be, and whether you would prefer to follow a rigorous screening schedule instead of making such a life-altering choice.
Whatever your decision, we encourage you to make an informed choice. If you do elect to have a preventive double mastectomy, our breast specialists will guide you in the appropriate breast surgery reconstruction to help restore your body image after treatment.
If you are interested in discussing ovary removal surgery , we will refer you to one of our gynecological oncologists.
Show me more…
Recommended Reading: Does Blue Cross Blue Shield Cover Bioidentical Hormone Therapy
Guidelines For Genetic Testing For Breast Cancer
About 10% of breast cancers are related to inheritance of damaged genes. BRCA1 and BRCA2 are the genes most frequently implicated, but there are many other genes, such as PALB2, ATM, and CHEK2, that need to be considered as well. Genetic testing usually starts with a family member who has already developed a breast or ovarian cancer. If this individual is positive for a mutation then all of the other family members can be tested for the same mutation to determine who is high risk and who is not. If no one in the family is known to carry a mutation then the test is considered non-informative. That means the test was unable to tell us which relatives in the family are high risk. People who have inherited a damaged gene are at increased risk for breast and other cancers. The risk may be as high as 80% depending on the specific gene and family history. Guidelines for determining whether an individual should get genetic testing or not are constantly evolving. General criteria include:
- Someone in your family is known to carry a mutated gene
- Ashkenazi Jewish ancestry
- You were diagnosed with breast cancer before age 50
- A man in your family has been diagnosed with breast cancer
- You were diagnosed with ovarian cancer
- There are multiple breast cancers on one side of your family
- Cancer was diagnosed in both breasts
Selective Estrogen Receptor Modulators And Breast Cancer
Knowledge about hormonal effects on breast cancer has expanded in the last three decades with the development of selective estrogen receptor modulators . This chemically diverse group of compounds involves a tertiary structure allowing them to bind to the estrogen receptor and to exert a specific set of agonist or antagonist effects on estrogen target tissues. Factors which influence agonist or antagonist activity in a given target tissue or circumstance include differences in estrogen receptor expression, receptor conformation on ligand binding and the expression of co-regulating proteins . SERM are particularly useful in breast cancer management because they offer possible treatment and prevention through estrogen antagonism coupled with the potential for useful estrogen agonist effects on normal tissues including bone, the cardiovascular system, and perhaps the central nervous system.
Tamoxifen is the most widely used SERM in the treatment of breast cancer tamoxifen and raloxifene are both used in prevention strategies. Both drugs have anti-estrogenic activity against breast cancer because they interfere with binding of the estrogen receptor to DNA structures, specifically by recruiting co-repressors that interact with the estrogen receptor at the estrogen response elements within target genes.
Recommended Reading: Nugenix Estro Regulator Review
Tests For Brca And Other Gene Mutations
A genetic test can tell you if you have any mutations in genes that are related to an increased risk of breast cancer. Its important to know that genetic testing is most helpful when you have a strong family history of either breast or ovarian cancer or a personal history of breast cancer.
If youd like to be tested, contact your doctor or your hospitals education office. Ask for a recommendation for a genetic counselor. Make an appointment and discuss the risks of undergoing genetic testing.
Your genes may affect your risk for breast cancer, but your lifestyle can have an impact as well. Whether or not you have a genetic mutation, its important to lower your risk whenever you can.
The following preventive measures may help you avoid a breast cancer diagnosis.
Breast Cancer Facts And Risk Factors
In this series
Most cases of breast cancer occur by chance. However, breast cancer does occur more often than usual in some families because of their genetic makeup.
In this article
Breast Cancer Facts and Risk Factors
In this article
Most cases of breast cancer occur by chance. However, breast cancer does occur more often than usual in some families because of their genetic makeup. Genetic means that the condition is passed on through families through special codes inside cells called genes. Your genetic ‘makeup’ is important because the material inherited from your parents controls various aspects of your body.
If you are concerned that your risk of developing breast cancer is higher than usual because of your family history then see your doctor for assessment.
If you have a moderately increased risk then an option is to have breast screening at an earlier age than normal and more often than usual. If you have a high risk then you may be offered genetic testing, counselling and regular breast screening tests.
Recommended Reading: Does Nugenix Have An Estrogen Blocker
Some Facts About Breast Cancer
- Breast cancer is one of the most common cancers in the world.
- In the UK about 1 in 8 women develop breast cancer at some stage of their lives.
- The biggest risk factor for developing breast cancer is increasing age. Most cases develop in women over the age of 50.
- Of women who do develop breast cancer, most do not have a strong family history of the disease. However, some women do come from families where breast cancer occurs more often than usual .
- If breast cancer is detected in an early stage, there is a good chance of a cure. X-ray testing of the breast can detect breast cancer at an early stage.
What Is Hereditary Cancer
Cancer arises from the uncontrolled growth of cells. Cancer is caused by harmful changes in the genetic messages which control the growth and division of cells which prevent them from being able to do their jobs effectively. We receive one complete copy of our genes from our mother and another from our father. It is the accumulation of multiple mutations over many years that disrupts the growth control of the cell and allows a normal cell to grow without control, and eventually become a cancer.
Most cases of cancer occur in the absence of a significant family history, and are not inherited. In these families the mutations causing the cancer occur only in the tumor itself and are all acquired after birth. Although the cause is seldom known, these acquired mutations may be the result of environmental or hormonal exposures, or mistakes which can occasionally occur when a cell divides. Acquired gene mutations cannot be passed from one generation to the next, so this type of cancer is considered “sporadic” and not hereditary. Just by chance, some families have several members affected with sporadic cancers.
Hereditary cancers generally are not significantly different from non-hereditary cancers. It is the way the cancers occur in the family that indicates whether they may be hereditary. Signs suggesting hereditary cancer include:
Don’t Miss: Can Having Your Tubes Tied Cause Hormonal Imbalance
Brca1 And Mammary Tumorigenesis In Animal Models
In animal models, loss of one Brca1 allele is not sufficient topromote cancer. For example, although homozygous deletions of Brca1 inknockout mouse models are lethal early in embryonic development, mice carrying heterozygous deletions of Brca1are phenotypically normal and do not exhibit an increasedpredisposition to tumorigenesis . However, when theremaining Brca1 gene is inactivated in mature heterozygousbrca1 knockout mice, mice will develop breast cancer.
Other Cancer Risks For People With Hboc
Anyone with mutations in the BRCA2 gene may be at an increased risk of other types of cancer, including melanoma and pancreatic, stomach, esophageal, and bile duct cancers.Mutations in other genes may be associated with an increased risk of developing breast and other cancers, including the Li-Fraumeni syndrome , Cowden syndrome, and others. The pattern of cancers in the family is often a clue to the specific gene that may explain the hereditary cancer for that family. Multigene panels are available for people with a strong personal and family history of cancer. Multigene panel tests include BRCA1 and BRCA2 and many other genes that increase the risk of breast, ovarian, and other cancers. If your BRCA1 and BRCA2 test was negative, then you may or may not have mutations in other genes. A newer type of testing, called next generation sequencing, massively parallel sequencing, or deep sequencing, has made testing for multiple genes at the same time faster and less expensive. If a genetic mutation is found, this could explain the cancers in a specific family and provide information about who is at risk and the appropriate types of monitoring and prevention/risk reduction methods.
Recommended Reading: How Long Does Olly Sleep Take To Work
What Causes Breast Cancer
Most breast cancers are caused by a combination of many different things
While the exact causes are still unknown, research has shown that some things can increase or decrease the likelihood of getting breast cancer. These are called ‘risk factors’. Being a woman and getting older are the biggest risk factors for developing breast cancer.
A small number of people have an increased risk of developing breast cancer because they have a significant family history. This may be because an altered gene that increases the risk of breast cancer runs in the family.
If you are worried about your family history you may be able to have a family history risk assessment.
Reproductive History Estrogen Is The Main Hormone Associated With Breast Cancer Estrogen Affects The Growth Of Breast Cells Experts Believe That It Plays An Important Role In The Growth Of Breast Cancer Cells As Well The Type Of Exposure And How Long Cells Are Exposed To Estrogen Affects The Chances That Breast Cancer Will Develop
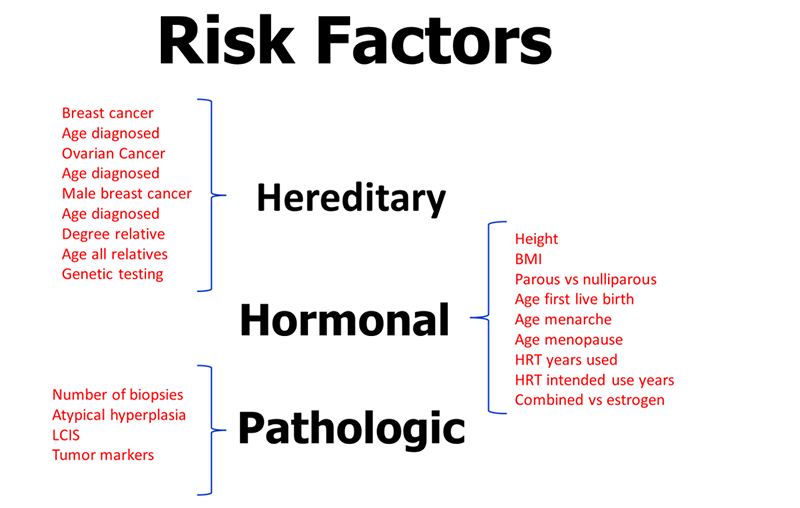
Early menarche
The start of menstruation is called menarche. Early menarche is when menstruation starts at an early age . Starting your period early means that your cells are exposed to estrogen and other hormones for a greater amount of time. This increases the risk of breast cancer.
Late menopause
Menopause occurs as the ovaries stop making hormones and the level of hormones in the body drops. This causes a woman to stop menstruating. If you enter menopause at a later age , it means that your cells are exposed to estrogen and other hormones for a greater amount of time. This increases the risk for breast cancer. Likewise, menopause at a younger age decreases the length of time breast tissue is exposed to estrogen and other hormones. Early menopause is linked with a lower risk of breast cancer.
Late pregnancy or no pregnancies
Pregnancy interrupts the exposure of breast cells to circulating estrogen. It also lowers the total number of menstrual cycles a woman has in her lifetime.
Women who have their first full-term pregnancy after the age of 30 have a slightly higher risk of breast cancer than women who have at least one full-term pregnancy at an earlier age. Becoming pregnant at an early age reduces breast cancer risk.
The more children a woman has, the greater the protection against breast cancer. Not becoming pregnant at all increases the risk for breast cancer.
Recommended Reading: Does Blue Cross Blue Shield Cover Testosterone Therapy
Histopathology And Molecular Features Of Familial Non
Very little is known about the genetic basis of non-BRCA1/2 breast cancer. Genetic linkage analysis of families has been performed and several chromosomal regions potentially harboring breast cancer susceptibility genes have been identified, including 8p12p22, 13q21, and 2q31q33. However, these loci have either been shown not to be major predisposing loci, or their status remains to be confirmed, thereby emphasizing genetic heterogeneity and population-specific effects among non-BRCA1/2 families. Non-BRCA1/2 hereditary carcinomas represent 67% of familial breast cancers when families with only female breast cancer and four or five affected members are considered. In the Spanish population, considering families with at least three cases of female breast cancer and one of the affected women being < 50 years, 75% of cases were not attributable to BRCA1/2 mutation.
There are three studies that have defined the histological characteristics of these neoplasias., , In the three studies, invasive ductal carcinoma was the most frequent histological type: 77% of the cases according to Lakhani et al, 78% in the series of Palacios et al and 67% in the study of Eerola et al. In two of them,, an excess of lobular carcinomas was found in familial non-BRCA1/2 compared with BRCA1 , BRCA2 , and sporadic cases . The difference was only significant with respect to BRCA1 tumors.
Does Breast Or Ovarian Cancer Run In Your Family
If you have close relatives with breast or ovarian cancer, you may be at higher risk for developing these diseases. Does your family health history put you at higher risk? Would you benefit from cancer genetic counseling and testing?
Each year, about 250,000 women in the United States are diagnosed with breast cancer and more than 20,000 are diagnosed with ovarian cancer. About 3% of breast cancers and 10% of ovarian cancers result from inherited mutations in the BRCA1 and BRCA2 genes that are passed on in families. Inherited mutations in other genes can also cause breast and ovarian cancer, but BRCA1 and BRCA2 are the genes most commonly affected. Although breast cancer is much more common in women, men with BRCA1 or BRCA2 mutations are more likely to get breast cancer than other men. BRCA mutations also increase the likelihood of getting pancreatic cancer and, in men, high grade prostate cancer. Knowing your family health history can help you find out if you could be more likely to develop breast, ovarian, and other cancers. If so, you can take steps to prevent cancer or to detect it earlier when it may be more treatable.
Don’t Miss: Can Having Your Tubes Tied Cause Hormonal Imbalance
Guidelines For Breast Cancer Screening
Breast cancer screening guidelines for average risk women have become confusing. One organization recommends that women start getting mammograms every other year at age 50 and another recommends yearly mammograms between age 45 and 55 with every other year mammograms thereafter. One reason for these differences is disagreement as to whether annual mammography in younger women can reduce the risk of dying of breast cancer. At Johns Hopkins, we continue to recommend annual mammography beginning at age 40 for average risk women,
Extra screening tests are recommended for women with higher than average risk for breast cancer. Current guidelines suggest that if you have more than a 20% risk of developing breast cancer during your lifetime you should consider adding screening breast MRI to your mammogram. Women who carry mutations in BRCA1, BRCA2, PALB2, or CHEK2 will meet this risk threshold. Other women with family history of breast cancer or a history of a breast biopsy showing high risk changes may meet this criterion as well. You can calculate your breast cancer risk online using the Gail model or the BCSC model . Breast specialists in the Johns Hopkins Breast Center have access to additional resources for calculating your breast cancer risk. At Johns Hopkins enhanced surveillance for high risk women consists of a breast exam every 6 months alternating mammograms with MRI scans.