Data Sources And Searches
MEDLINE , the Cochrane Library, and EMBASE were searched for English-language articles published from January 1, 2016, through October 12, 2021 . Targeted searches were conducted for unpublished literature . Additional citations were identified through review of pertinent review articles and of literature suggested by peer reviewers or public comment respondents.
Between October 2021 and July 2022, ongoing surveillance through article alerts and targeted searches of selected journals was conducted to identify major studies possibly affecting the USPSTF recommendation.
Is Hormone Replacement Therapy Safe
When used under medical supervision and on a temporary basis, hormone replacement therapy has been proven safe. Studies indicate that women and men on HRT experience a decreased risk of osteoporosis and colon cancer. Individuals who are involved in HRT have seen overall improvements in muscle tone, weight gain and overall physical and emotional health.
Tissue Selective Estrogen Complex
TSECs pairs a selective estrogen-receptor modulator with estrogen. The FDA approved medication marketed as DuaVee combines 20 mg bazedoxifene, a selective estrogen-receptor modulator, with 0.45 mg oCEE for use in postmenopausal women with a uterus. It is used for moderate to severe VMS and for prevention of osteoporosis. Compared to placebo, TSEC had a similar profile in that it did not increase breast tenderness, breast density, or endometrial thickness avoiding these conditions may be indications to use this therapy over other formulations. Amenorrhea occurs in more than 83% of users . It has not been studied regarding its ability to provide breast cancer risk reduction.
Recommended Reading: How To Get Rid Of Hormonal Belly
Added Benefits Of Hrt
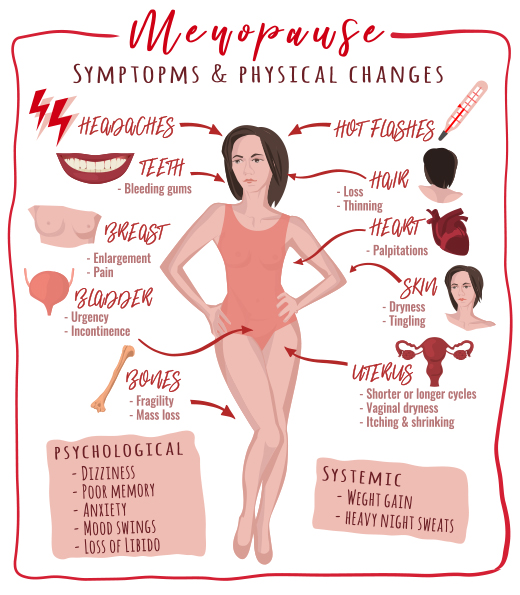
HRT reduces the risk of various chronic conditions that can affect postmenopausal women, including:
- diabetes taking HRT around the time of menopause reduces a womans risk of developing diabetes
- osteoporosis HRT prevents further bone density loss, preserving bone integrity and reducing the risk of fractures, but it is not usually recommended as the first choice of treatment for osteoporosis, except in younger postmenopausal women
- bowel cancer HRT slightly reduces the risk of colorectal cancer
- cardiovascular disease HRT has been shown to reduce cardiovascular disease markers when used around the time of menopause.
Breast Cancer And Hrt
Women over 50 years of age who use combined oestrogen and progestogen replacement for less than five years have little or no increased risk of breast cancer. Women who use combined HRT for more than five years have a slightly increased risk. Women on oestrogen alone have no increased risk up to 15 years of usage.
There is no evidence to suggest that a woman with a family history of breast cancer will have an added increased risk of developing breast cancer if she uses HRT. The risk with combined oestrogen and progestogen is greater than with oestrogen alone, or with newer HRT agents such as tibolone , and may also depend on the type of progestogen used. Studies suggest that medroxyprogesterone acetate and norethisterone have higher risks than dydrogesterone and progesterone.
You May Like: Does Estrogen Help With Hair Loss
Where Does Evidence About The Health Effects Of Mht Come From
The most comprehensive evidence about the health effects of MHT comes from two randomized clinical trials that were sponsored by the National Institutes of Health as part of the Womens Health Initiative :
- The WHIEstrogen-plus-Progestin Study, in which women with a uterus were randomly assigned to receive either a hormone pill containing both estrogen and progestin or a placebo. The median duration of treatment was 5.6 years.
- The WHI Estrogen-Alone Study, in which women without a uterus were randomly assigned to receive either a hormone pill containing estrogen alone or a placebo. The median duration of treatment was 7.2 years.
More than 27,000 healthy women who were 50 to 79 years of age at the time of enrollment took part in the WHI hormone therapy trials. The goals of these trials were to see if MHT prevents heart disease and bone fractures in postmenopausal women and to determine if MHT affects risks of breast cancer and, for women with a uterus, endometrial cancer. Both trials were stopped early , when it was determined that both types of therapy were associated with specific health risks, but long-term follow up of the participants continues to provide new information about the health effects of MHT.
Venous Thrombosis And Hrt
Venous thromboses are blood clots that form inside veins. Women under 50 years of age, and women aged 50 to 60, face an increased risk of venous thrombosis if they take oral HRT. The increase in risk seems to be highest in the first year or two of therapy and in women who already have a high risk of blood clots. This especially applies to women who have a genetic predisposition to developing thrombosis, who would normally not be advised to use HRT.
Limited research to date suggests the increased risk of clots is mainly related to combined oestrogen and progestogen in oral form, and also depends on the type of progestogen used. Some studies suggest a lower risk with non-oral therapy or tibolone.
You May Like: How To Deal With Hormonal Mood Swings
Can Increase The Risk Of Blood Clots
Studies have shown that HRT may raise your risk of blood clots and stroke. This risk may be highest for people over 60 or who started menopause over a decade ago. The longer you take HRT, the greater the increase in your risk.
Because of this risk, health experts recommend the lowest possible HRT dose for the shortest period of time for people over 60 or who are 10 years past the onset of menopause.
Here Are Some Questions You Can Ask Yourself And Discuss With Your Physician:
- Am I experiencing difficult menopause symptoms?
- Do I have any medical conditions or a family history of certain conditions that might make HRT beneficial for me?
- Do I have any medical conditions or a family history of certain conditions that might make HRT riskier for me?
- Have I considered alternatives to HRT?
Read Also: Which Is Better Testosterone Gel Or Injections
Choosing The Right Hrt For You
It is important to find the correct HRT to help your symptoms.
A low dose of HRT hormones is usually prescribed to begin with. If you need to, you can increase your dose at a later stage.
Once youâve started HRT, itâs best to take it for a few months to see if it works well for you. If not, you can try a different type or increase the dose. Itâs really important that you talk to your GP if you have any problems with HRT.
How Can I Reduce These Side Effects Of Hormone Therapy
In most cases, these side effects are mild and dont require you to stop your HT. If your symptoms bother you, ask your healthcare provider about adjusting either the dosage or the form of the HT to reduce the side effects. Never make changes in your medication or stop taking it without first consulting your provider.
Recommended Reading: How To Help Hormonal Imbalance Naturally
The Health Risks And Benefits Of Hrt
In 1991, the U.S. National Institutes of Health launched the Women’s Health Initiative , a set of studies involving healthy post-menopausal women that was carried out in 40 U.S. centres. The WHI included a clinical trial to evaluate the risks and benefits of the two types of HRT and to see how they affected the incidence of heart disease, breast cancer, colorectal cancer and fractures in post-menopausal women. The trial was divided into two arms:
- One arm involved more than 16,000 post-menopausal women aged 50 to 79 who had not had a hysterectomy. They took pills daily that were either a combination of estrogen and progestin , or a placebo .
- The second arm involved more than 10,000 women who had received a hysterectomy and who took estrogen pills alone or a placebo.
In July 2002, after an average 5.2 years of regular follow-up, the NIH prematurely ended the combined HRT arm of the WHI trial. An independent monitoring board, which regularly reviewed the findings, concluded that there were more risks than benefits among the group using combined HRT, compared with the placebo group. The study found that changes in the incidence of disease per 10,000 women on combined HRT in one year were:
- Seven more cases of coronary heart disease
- Eight more cases of strokes
- Eighteen more cases and a twofold greater rate of total blood clots in the lungs and legs
- Eight more cases of invasive breast cancer
- Six fewer cases of colorectal cancer
- Five fewer cases of hip fractures
Do Local Formulations Of Menopausal Hormone Therapy Have Different Risks

Both systemic and local treatment options for MHT are available in the United States. Which option a woman receives depends on the menopausal symptoms the treatment is meant to address. Systemic MHT is usually prescribed to treat hot flashes and to prevent osteoporosis. Systemic MHT with combined estrogen plus progestin or with estrogen alone can be given as oral medications as transdermal patches, gels, or sprays and as implants.
Local MHT is prescribed to treat genitourinary symptoms such as vaginal dryness. Local MHT contains low-dose estrogen only and is prescribed to women regardless of their hysterectomy status. Local MHT with low-dose estrogen alone includes creams, tablets , and rings.
Findings from the Womens Health Initiative Observational Study showed that, among women with an intact uterus, those who used vaginal estrogen and those who didnt had similar risks of stroke, invasive breast cancer, colorectal cancer, endometrial cancer, and pulmonaryembolism/deep vein thrombosis .
Read Also: Phexxi Non Hormonal Birth Control
Are There Alternatives For Women Who Choose Not To Take Menopausal Hormone Therapy
Women who are concerned about the changes that occur naturally with the decline in hormone production that occurs during menopause can make changes in their lifestyle and diet to reduce the risk of certain health effects. For example, eating foods that are rich in calcium and vitamin D or taking dietary supplements containing these nutrients may help to prevent osteoporosis. FDA-approved drugs such as alendronate , raloxifene , and risedronate have been shown in randomized trials to prevent bone loss.
Medications approved by the FDA for treating depression and seizures may help to relieve menopausal symptoms such as hot flashes . Drugs that have been shown in randomized clinical trials to be effective in treating hot flashes include venlafaxine , desvenlafaxine , paroxetine , fluoxetine , citalopram , gabapentin , and pregabalin.
Harms Of Menopausal Hormone Therapy
Key Question 2. What are the harms of menopausal hormone therapy when used for the primary prevention of chronic conditions?
Estrogen Only
Women receiving estrogen-only therapy had statistically significant increases in risk for gallbladder disease, stroke, urinary incontinence, and venous thromboembolism . Increased risks did not persist after stopping hormone therapy.
The Postmenopausal Estrogen/Progestin Interventions Trial 29 and the WHI 40 reported increased risks for gallbladder disease in women receiving estrogen-only therapy. In the WHI, the increased risk was statistically significant .
Of 3 trials assessing the risk of stroke , only the WHI provided statistically significant results. Estrogen-only therapy led to a statistically significant increase in risk for stroke .
Two trials with data on more than 3200 continent women found higher risks of urinary incontinence in the treatment groups for all time points .
Based on the WHI results,15 women randomized to estrogen-only therapy had a statistically significant increase in risk of venous thromboembolism compared with those randomized to placebo .
To balance benefits and harms, the WHI used a global index based on beneficial and harmful events. For estrogen-only therapy, the global index did not show a statistically significant difference in overall beneficial or harmful events .
Estrogen Plus Progestin
You May Like: Natural Ways To Cure Hormonal Acne
Taking Estrogen With A Progestin Vs Estrogen Alone
Treating menopausal symptoms with estrogen and progestin together is known as estrogen-progestin therapy or combined hormone therapy. Although estrogen alone improves the symptoms of menopause, it increases the risk of cancer of the uterus . Adding a progestin to the estrogen lowers the risk of endometrial cancer back to normal. Because of this, EPT is given to women who still have a uterus . EPT can be given 2 ways:
- Continuous EPT means the same dose of estrogen and progestin is taken each day. Women often prefer continuous EPT because it rarely leads to menstrual-like bleeding.
- Sequential EPT means different amounts of each hormone are taken on specific days. There are different ways to do this. For example, estrogen can be taken by itself for 14 days, then estrogen plus progestin for 11 days, then neither hormone for 3 to 5 days. Other schedules involve taking progestin only every few months. This lowers the amount of progestin that you are exposed to. Monthly regimens are also thought to result in hormone levels that are more like the natural menstrual cycle. Cyclical EPT can produce bleeding like a menstrual period, but it can occur less often than monthly.
Difference In Benefits And Harms By Subgroup
Key Question 3. Do the benefits and harms of menopausal hormone therapy differ by subgroup or by timing of intervention ?
Subgroups
Trials did not report results for most of the subgroups. Subgroup analyses were restricted to age, race/ethnicity, and a limited number of comorbidities or risk factors. In general, tests of interactions did not detect any statistically significant subgroup effects for most outcomes of interest. An exception is the interaction with age. Analyses that compared younger with older women using estrogen-only therapy yielded statistically significant trends for increasing risks by age for myocardial infarction ,15 colorectal cancer ,15 and all-cause mortality .15 Such subgroup differences, however, are based on relatively few events and should be interpreted cautiously. For example, only 48 women in the 50- to 59-year-old age group experienced a myocardial infarction. eTable 19 in the Supplement presents the strength of evidence for subgroup results.
Also Check: Where To Buy Melatonin For Dogs
Benefits And Risks Of Menopause Hormone Therapy
Estrogen is the most effective treatment for VMS. Women with an intact uterus require combined progestogen therapy with estrogen for endometrial protection. For those without a uterus, estrogen alone can be used. Since the risk-benefit profile of HT treatment in symptomatic menopausal women is impacted by age, time since menopause and existing comorbidities, shared decision making is critical in determining what HT formulation and route to use and when discontinuation is appropriate . Table 3 summarizes the evidence on risks and benefits of HT.
Types Of Studies Of Hormone Therapy And Cancer Risk
Different types of studies can be used to look at cancer risk from menopausal hormone therapy .
Randomized controlled trials: In this kind of study, a group of patients get the drug being studied , and another group gets a placebo . Results from this kind of study are powerful because which group a patient is in is based on chance. This helps assure that the groups are similar in all ways, such as risk for cancer, except for the drug thats being studied. This is the best way to see the effects of a drug. These types of studies can also be double-blinded, which means neither the people in the study nor their doctors know which group they are in. This lowers the chance that thoughts or opinions about treatment could affect the study results. Unfortunately, these kinds of studies are costly, which limits the number of people in the study, how long the study can continue, and the number of studies done.
A major drawback of observational studies is that the people getting the treatment being studied may have different cancer risk factors than the people who arent. Plus, the treatment can differ between the people being studied. This makes it less clear that the differences seen are only due to the drug being studied and not other factors.
When observational studies and randomized controlled trials have different results, most experts give more weight to the results of the randomized controlled trial.
Recommended Reading: How To Measure Your Testosterone
When Hrt Is Not Recommended
Hormone replacement therapy is notrecommended for people who:
- May be pregnant
- Have issues with abnormal vaginal bleeding
- Have a family or personal history of breast cancer
- Have a personal history of heart disease, stroke, blood clots, or liver disease
- Have a family history of gallbladder disease
- Are allergic to estrogen or progesterone
Benefits And Harms Of Hormone Therapy By Subgroup And Timing Of Intervention
Key Question 3. Do the benefits and harms of menopausal hormone therapy when used for the primary prevention of chronic conditions differ by subgroup or by timing of intervention?
Subgroups
Subgroup analyses were restricted to age, race and ethnicity, oophorectomy status, and a limited number of coexisting conditions or risk factors in the WHI. In general, tests of interactions did not detect any statistically significant subgroup effects for most outcomes of interest. An exception is the interaction with age, which was a prespecified subgroup analysis in the WHI.
Analyses that compared younger and older persons using estrogen-only therapy yielded statistically significant trends for increasing risks by age for myocardial infarction , colorectal cancer , and all-cause mortality .16 The significant interaction of colorectal cancer and all-cause mortality with age was no longer present with extended follow-up of 13 to 18 years.
Subgroup differences, however, are based on relatively few events and should be interpreted cautiously. For example, only 48 persons in the 50- to 59-year-old age group experienced a myocardial infarction.
Timing of Intervention
These results pertain to persons who use hormone therapy for the purpose of preventing chronic conditions. They do not pertain to persons who use hormone therapy for the management of menopausal symptoms, which requires different consideration and weighing of benefits and harms.
You May Like: What Does Low Testosterone Do