The Biote Method Of Bioidentical Hormone Replacement Therapy
- The Biote Method of hormone optimization is the result of condensing over 80 years of scientific research into a program that may help with the earliest signs of aging.
- The Biote Method uses pellets, which are about the size of a grain of rice, for hormone optimization. Your provider at AWC Wellness and Aesthetics inserts these tiny pellets under the skin during a simple, in-office procedure.
- The pellets will then dissolve slowly over time they only need to be re-administered approximately every 3-5 months, depending on the patient.
- As the pellets dissolve, they release a steady stream of hormones into your bloodstream, and will ultimately be completely absorbed, leaving nothing behind.
Other Factors Beyond Menopause
Menopause is not the only consideration, when looking for a cause of urinary incontinence. The following factors can play a role in your risk of UI:
Drinking alcohol and carbonated or caffeinated drinks, like coffee or tea fills your bladder quickly and may make you feel like you need to use the bathroom more often.
Drinking in the evenings can necessitate frequent trips to the bathroom and leaking throughout the night.
Not eating enough fiber can lead to constipation, which adds stress to the pelvic floor.
Extra weight, especially around the abdomen, increases pressure over the bladder.
Infections in the urinary tract can cause UI, but after treatment, this should improve.
Taking certain medications like steroids and diuretics can result in UI.
Nerve damage can interfere with the signals between the bladder and brain, creating a situation where you leak because you dont feel any urge to urinate.
Treatments For Associated Conditions
POI is associated with other health conditions, including Addison’s disease, Fragile X permutation, thyroid dysfunction, depression, anxiety, and certain other genetic, metabolic, and autoimmune disorders.
Women who have POI as well as one of these associated conditions will require additional treatment for the associated condition. In some cases, treatment involves medication or hormone therapy. Other types of treatments might also be needed.
Also Check: How Do You Get Estrogen
Evaluation Of Other Outcomes
It is also pertinent to comment upon the findings related to breast cancer risk in both the WHI and GPRD studies. As shown in figure 1, breast cancer was increased in both the older and younger women treated with combined HT in the GPRD studies, similar to the findings in the WHI RCT. Furthermore breast cancer risk was unchanged in both the older and younger women with a prior hysterectomy treated with estrogen only in the GPRD studies, similar to the results in the WHI RCT. Additional analyses of women in both the combined HT and estrogen only GPRD studies that were not exposed to HT at any time prior to the start of the study, yielded results for breast cancer similar to the overall study cohorts.
As reported in our primary publications other outcomes, including colorectal cancer and hip fracture, largely were similar in the GPRD and WHI studies for both the comparisons of combined HT and estrogen only therapy . Venous thromboembolic events also were similar in the studies of combined hormonal therapy, but probably suffered from unmeasured confounding in the GPRD estrogen-only study, as was found for myocardial infarction and CVA.
To Reap Benefits Of Hormone Replacement Therapy Sooner Is Better
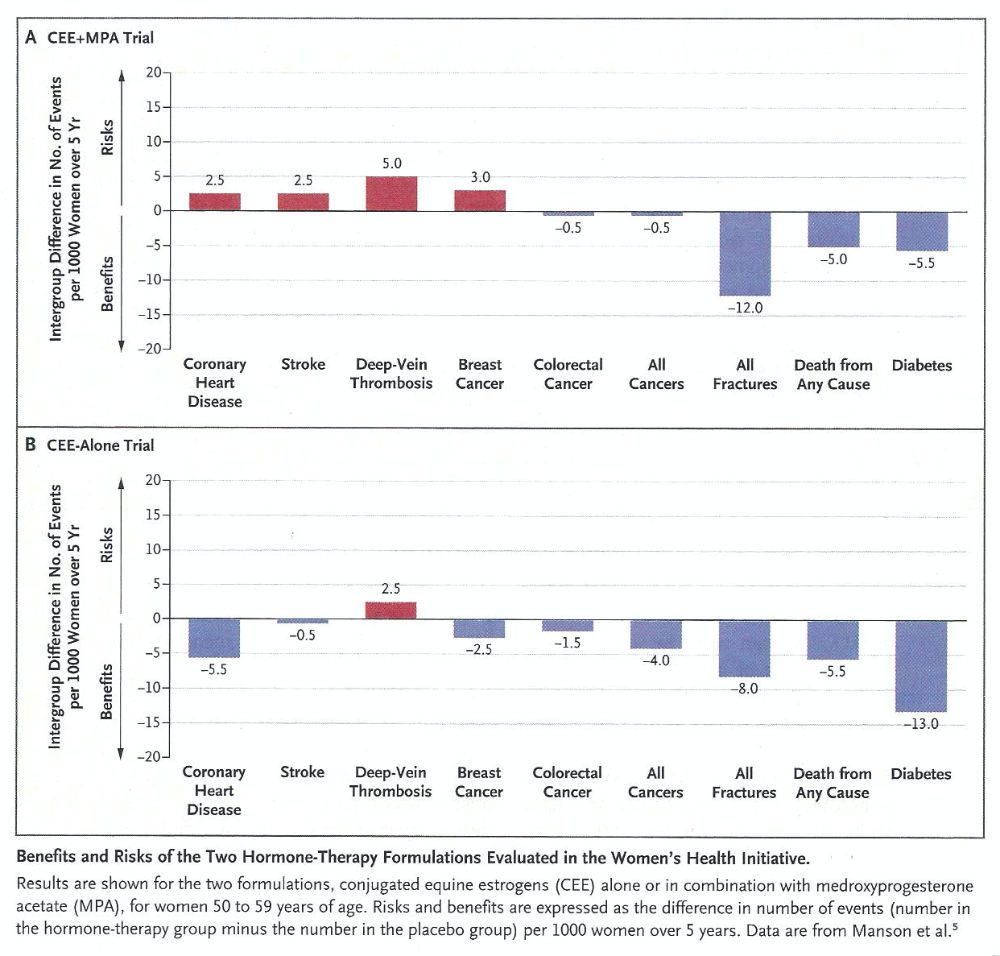
The studies that found hormone therapy lowered the risk of heart attack involved tens of thousands of women between the ages of 35 and 55. They started to take the medication when they first began to feel uncomfortable or as they reached menopause. In the Womens Health Initiative study, though, the investigators tested a much older population with an average age of 63. Thats more than a decade after women typically reach menopause.
This led to a new idea: The therapy might protect heart health with less risk of breast cancer if women take it before they turn 60.
For hormone therapy to slow down heart disease, a womans blood vessels need to be clean and healthy, Hodis says. If vessels are already diseasedwhich can happen once women are well beyond menopauseestrogen wont help much.
Women who started hormone therapy within six years of menopause had less hardening of their arteries.
Hodis and his colleagues investigated this theory in a study that included hundreds of healthy postmenopausal women. Their results in 2016showed promise. Women who started hormone therapy within six years of menopause had less hardening of their arteries, known as atherosclerosis, and that translates to lower heart attack and stroke risk. But it didnt help women in the study who were already 10 years past menopause.
Researchers are still trying to understand why hormone therapy is more effective in women closer to menopause, but Hodis has a theory.
Don’t Miss: How Can I Get Female Hormones
Additional Analyses Conducted In The Two Trials
Women without pre-randomization use of hormone therapy
Approximately one quarter of estrogen-progestin and one half of estrogen-alone trial participants had used HT pre-randomization. To simulate first initiation of HT in clinical practice, secondary analyses were conducted in women without pre-randomization HT use, stratified by age group . The age-stratified findings remained similar to the primary analysis for CEE+MPA, but were slightly more favorable for younger women in the CEE trial. Among women aged 5059 without prior HT use, the global index was significantly better for those assigned CEE compared to placebo , with 40 fewer adverse events per 10,000 pys in the CEE group, compared to 34 excess events per 10,000 pys among women aged 7079.
Analyses stratified by presence or absence of vasomotor symptoms at baseline
Sensitivity analyses censoring for noncompliance with study pills
Secondary analyses among adherent women were generally similar to intention-to-treat results but tended to accentuate the findings in each trial. For example, the intervention-phase adherence-adjusted HR for CHD was 1.32 in the CEE+MPA trial and 0.85 in the CEE trial, while the HR for breast cancer was 1.52 in the CEE+MPA trial and 0.58 in the CEE trial.
Other analyses
What Is The Goal Of The Whi
The Women’s Health Initiative , sponsored by the National Heart, Lung, and Blood Institute , is a long-term national health study that focuses on strategies for preventing heart disease, breast and colorectal cancer, and osteoporosis in postmenopausal women. These chronic diseases are the major causes of death, disability, and frailty in older women of all races and socioeconomic backgrounds.
The original WHI study had three partsa clinical trial, an observational study, and a community prevention studyand completed data collection in 2005. The WHI continues to contribute to the science of womens health through extension and ancillary studies.
WHI extension studies collect long-term data from WHI participants to complement the original WHI study. The current extension study is collecting annual health information from consenting WHI participants through 2020, focusing on cardiovascular events and aging.
WHI ancillary studies are separate research projects that enroll WHI participants. Examples include:
Recommended Reading: How To Naturally Increase Testosterone In Women
Subgroup Analysis Based On Hormone Use
Analysis was performed based on category of experience with HT use into never-users, former users , quitters , restarters , and continuers . Six questionnaires had missing or contradictory responses precluding determination of whether they were former users or quitters. Characteristics of these subgroups are displayed in Table .
Table 2 Characteristics of Respondents by Category of HT Use Experience
There were 43 respondents who were not using HT in July 2002. Never-users were largely represented by the vindicated belief pattern. Some described personal medical reasons for not using. Former users sometimes gave reasons for stopping based on side effects of HT. Also in this group were women who used HT for a while based on physician recommendation, though never comfortable with the idea. Others stopped because they had no perceived need to continue.
Recent quitters were a highly symptomatic and concerned group. “My hot flashes have returned with nearly the same intensity they were when I first started using hormones. I am consulting with my doctor now to find out what my options are.” “I miss the effects of estrogen positive attitude, more energy, higher metabolism and sex drive.” “I am not taking hormones now solely because I fear the side effects, I felt much better when I was taking them.” Some women were considering restart.
Is It Safe For Women With Poi To Take Hrt
In general, HRT treatment for women with POI is safe and is associated with only minimal side effects. Women with POI take HRT to replace hormones their bodies would normally be making if they didn’t have POI.
The HRT taken by women with POI is different from the hormone therapies taken by women who are going through or have gone through natural menopause, which are often called menopausal or post-menopausal hormone therapy .
A large, long-term studycalled the Women’s Health Initiativeexamined the effects of a specific type of PMHT, taken for more than 5 years, by women ages 50 to 79 who had already gone through menopause. This study showed that PMHT was associated with an increased risk of stroke, blood clots, heart disease, heart attacks, and breast cancer in these women.11
These results do not apply to young women with POI who take HRT.3,10 The type and amount of HRT prescribed to women with POI is different from the PMHT taken by older women.3
A woman should talk to her healthcare provider if she has questions about HRT as a treatment for POI. Also, she should tell her healthcare provider about any side effects she experiences while taking HRT. There are many different types of HRT. Women should work with their healthcare providers to find out the best type of treatment.
Also Check: Supplements To Balance Hormones And Lose Weight
Cost Effectiveness Of Ht
Assessments of quality-adjusted years of life in women on HT have consistently shown that HT is cost-effective, predominantly in younger women . In The Endocrine Society Task Force report on HT, the number of younger women benefiting from the reduction in symptomatology greatly overcomes numerically any of the attributable risks or benefits discussed above .
Attributable or excess risk or benefit per 1000 women receiving menopausal HT for 5 years who are 5059 years old or < 10 years from menopause who have relief from hot flushes and symptoms of vaginal atrophy.
Shortcomings Of The Whi And Mws Studies And Their Findings
The publication of these results triggered an immediate response from experts through the British Menopause Society, the International Menopause Society and others, who considered that both the WHI and the MWS studies had shortcomings and so were flawed.
Issues with the studies:
Womens Health Concern also expressed its concern at that time, wanting to ensure that decisions on HRT usage were based on fact. Today it is important that the medical profession and the media do not create the impression that these flawed studies should significantly influence a womens decision making about HRT which they should not.
Also Check: How To Get Your Hormones Balanced Naturally
Lower Doses Of Hormone Therapy
Research findings show that lower doses of EPT and ET relieve vasomotor symptoms, prevent vaginal atrophy, are associated with a reduced incidence of endometrial bleedingespecially in the early months of therapyprovide effective endometrial protection, and prevent early postmenopausal bone loss.13,14,15,16 These lower-dose options provide clinicians and patients with expanded options for individualizing ET/EPT.
The Million Women Study
- From 1996 to 2001
- One million women in the UK who were attending breast screening clinics as part of the NHS Breast Screening Programme were surveyed by questionnaire
- Participating women were over 50 years old
- Looked at the risks of breast cancer and other health issues in HRT users compared with non-users in a total of 828,923 women.
- Estrogen-only HRT causes a small increase in the risk of breast cancer
- Estrogen-only HRT causes a small increase in the risk of womb cancer
- Estrogen-only HRT causes a small increase in the risk of ovarian cancer
- Combined HRT increases the risk of breast cancer more than estrogen-only HRT
- Combined HRT reduces the risk of womb cancer
- The longer HRT is used, the higher the risk of breast cancer
- The risk of breast cancer disappears as soon as HRT is stopped
- No increased risk of venous thrombosis with transdermal estrogen.
2020: The WHI long term randomised clinical trials was published and reported breast cancer incidence and mortality on 27,000 women followed up until 2017. It reported that women using estrogen only HRT had a reduced risk of breast cancer incidence and mortality but those on combined HRT had a slight increased risk of breast cancer incidence. Importantly, this did not translate into an increased risk of mortality.
They also reported on an increased risk of invasive breast cancer and breast cancer mortality in obese women.
Read Also: Benzoyl Peroxide For Hormonal Acne
Whi Research Changes Therapies Saves Lives
In 2002, 5 million postmenopausal women in the U.S. were using combination hormone replacement therapy to alleviate the symptoms of menopause and prevent fractures and heart attacks. However, research conducted by the WHI found a direct link between combination HRT and increase in heart disease, stroke and breast cancer.
The WHI findings singularly changed the face of women’s medicine around the world. Researchers estimate that the subsequent decrease in the use of combination HRT resulted in a significant reduction in breast cancer cases in several countries and reduced rates of heart attack and stroke in the U.S.
Fred Hutchinson Cancer Center is an independent organization that serves as UW Medicine’s cancer program.
Whi Study Announced And Planning Begins
On April 19, 1991, Dr. Bernadine Healy, newly appointed as the first female director of the NIH, announced her plan for the Women’s Health Initiative . Planning for the WHI CT/OS study began that year. In order to promote cross-institutional collaboration, and to prevent the loss of funding to other women’s health-related studies, funding was requested and obtained directly from Congress in the form of a discrete line item, with a projected budget of $625 million over the life of the 15-year study.
The NIH awarded the role of Clinical Coordinating Center to the Fred Hutchinson Cancer Research Center , located in Seattle, Washington. The CCC’s responsibilities included the coordination of the 40 study clinics that would eventually recruit women nationwide, as well as ensuring their consistent adherence to the study design and guidelines.
Recommended Reading: Does Melatonin Increase Deep Sleep
Phytotherapy An Effective Alternative To Hrt
Phytotherapy, the use of medicinal plants and plant extracts heal and restore balance in the body, is a great way to manage menopause symptoms without the risks of HRT. Several herbs have shown great results for women. We recommend black cohosh, kudzu, and red clover for symptoms of estrogen imbalance like hot flashes and night sweats. Passionflower, chasteberry, and wild yam work well for symptoms related to progesterone imbalance like anxiety, insomnia, and irritability.
Weve found that the most effective approach to eliminating menopause symptoms includes a multi-botanical like our Herbal Equilibrium , plus a high-quality multivitamin/mineral complex and hormone-friendly changes in diet and lifestyle. Our Hormonal Health Program includes all of this, plus phone support from women right here in Maine so you can personalize our approach to fit your needs for menopause relief. There are lots of options for frustrating menopause symptoms and we are here to help!
Whi Study Antecedents And Demonstration Of Feasibility For A Large
Among postmenopausal women, cardiovascular disease, cancer, and osteoporosis are the leading causes of morbidity and mortality, as well as impaired quality of life. Among women in all age groups, cancer and cardiovascular disease are the leading causes of mortality. As the incidence of these diseases increases according to age, women over the age of 50 bear much of the disease burden.
It had been generally accepted that postmenopausal estrogen deficiency may play a role in these morbidities, and that dietary, behavioral, and drug interventions may forestall their development. However, these findings were identified on the basis of epidemiologic observational studies alone. Such interventions would require testing through clinical trials before they, along with their full range of risks and benefits, could be used as the basis for setting public health policy and creating prevention guidelines.
However, concerns existed about the feasibility of such a complex clinical trial among participants in this demographic of older women, particularly with respect to sufficient recruitment and adherence to the dietary and hormone-treatment regimens.
Read Also: Are There Any Side Effects From Melatonin
Study Organization And Implementation
Given the complexity of the WHI study, both in terms of the number of interventions and outcomes studied, as well as the number and geographic distribution of participants and clinical centers, careful orchestration was required. To this end, the WHI maintained a carefully designed organizational structure, along with governance- and science-specific committees and communications channels for staff and investigators to resolve study-related questions and exchange information. As the study launched concurrently with the early stages of modern Internet connectivity, the study centers had to be supplied with computing and networking equipment to connect to the WHI network WHI-hosted e-mail facilitated the efficient exchange of information among staff and scientists, as well as the transfer of study-related data.
The launch of the study was undertaken in two stages. At first, 16 “vanguard” study centers entered active operation, to evaluate the study protocol and procedures. Once this initial portion of the study was underway, the remaining 24 study centers entered the study around a year later, each assigned to one of the “vanguard” study centers for purposes of mentorship. Study centers were subdivided into four regions, each under the supervision of a regional center, to further facilitate communication and information exchange among study centers.