Great Weight Loss Program
I came to see Dr. Inna because I was in the worst physical shape of my life, morbidly obese, weighing 280 lb. I felt tired, unhappy, lacked energy, and struggled with shortness of breath and persistent psoriasis outbreaks. My multiple previous weight loss projects failed, so I was quite skeptical. But this time it was different because of the whole program and mentoring I have received from Dr. Inna. I now have knowledge and tools to maintain these results for life. I have lost 89 pounds, I am no longer obese, and feel fantastic. I havent had a flare of psoriasis since I started the program. My blood pressure is under control. I have my energy back. My family and coworkers noticed a dramatic difference. My daughter and I enjoy our time together, she means the world to me. I want to be there for her for a long time. And I know I will be a super Granddad to my grandkids one day, because I will be physically capable. Dr. Inna literally guided me to re-create MY health, for which I am forever grateful. I wholeheartedly recommend this program to anyone who wants to live a long and healthy life.
Natural Solutions For Dryness
At menopause, vaginal blood flow falls. Dryness and irritation can occur, and bacteria infections that pass to the urinary tract are more likely.
What is to be done? First of all, even after the ovaries stop, the adrenal glands and the fat tissue continue to contribute to estrogen production after menopause. In addition, phytoestrogens in plants provide weak estrogen effects. Soy products, such as tofu, tempeh, and miso, contain huge amounts of these natural compounds.
The plant-derived estrogen and progesterone creams described above can be helpful. Used on a regular basis, these creams maintain a moist vaginal lining. However, please note that they should not be used as a sexual lubricant. Estrogen cream is a medication, not a lubricant, and it goes through any skin it touches, including mens. Many women prefer to avoid hormone creams entirely and use ordinary lubricants or moisturizers instead.
Cardiovascular Issues And Menopause
Coronary artery disease is the leading cause of morbidity and mortality in men and postmenopausal women. Menopause increases the risk for women still further, independent of age. Before menopause, the risk of CAD for women lags behind the risk for men by approximately 10 years after menopause, it catches up. As a result, mortality from CAD is increasing in women. The Framingham study was pivotal in showing the relation between menopause and increased cardiovascular mortality.
The Womens Health Initiative was a randomized, controlled trial that addressed the issue of whether postmenopausal women should take hormone therapy or estrogen therapy for prevention of CAD more than 27,000 healthy women participated in the trial. The investigators concluded that hormone therapy and estrogen therapy are not indicated for the prevention of CAD.
Emerging analyses of WHI data from the Estrogen-Alone Triala double-blind, placebo-controlled, randomized clinical trial evaluating the effects of conjugated equine estrogens on chronic disease incidence among postmenopausal women with prior hysterectomy and after a mean of 7.1 years of follow-upsuggested that treatment effects differ by age. Compared with older women, younger women receiving CEE had a lower risk of CAD.
Also Check: Can You Get Pregnant On Hormone Replacement Therapy
Testing Perimenopause And Menopause Hormone Levels: Is It Worth It
We see the numbers a lot: estradiol, estrogens, FSH. But what do they mean, and what can they actually tell a woman about where she is in the menopause transition?
Turns out, the team at Gennev found that using a menopause hormone levels chart may be less helpful than weâd like.
While there are uses for having hormone levels tested, pinpointing your place on the perimenopause-to-menopause journey probably isnât one of them. Hormones just donât cooperate during this time , and hormone tests can only really offer a limited snapshot of where you are right now â which is probably not where youâll be tomorrow.
To understand all this better, we had a Q & A with our ob/gyn Chief Medical Officer, Dr. Rebecca Dunsmoor-Su, on to test or not to test.
Potential Role In Vascularization Of Solid Tumors
Elevated FSH receptor levels have been detected in the endothelia of tumor vasculature in a very wide range of solid tumors. FSH binding is thought to upregulate neovascularization via at least two mechanisms one in the VEGF pathway, and the other VEGF independent related to the development of umbilical vasculature when physiological. This presents possible use of FSH and FSH-receptor antagonists as an anti-tumor angiogenesis therapy .
You May Like: How To Care For Hormonal Acne
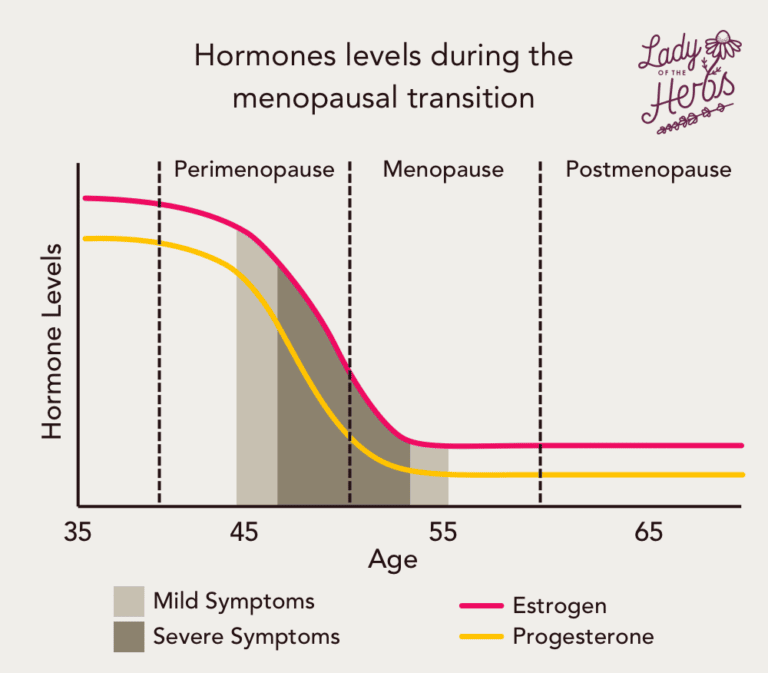
The Cycle And Stages Of Hormone Changes During Menopause
Throughout their reproductive years, women undergo hormonal changes on a monthly basis. They include fluctuations in estrogen, progesterone, luteinizing hormone , and follicle stimulating hormone . These hormones play a role in regulating the menstrual cycle and maintaining pregnancy, should it occur.
As a woman approaches menopause, this monthly cycle becomes less regular. Furthermore, the overall levels of these hormones begin to change.
Experts consider there to be four distinct stages of perimenopause and menopause. These are listed below with their corresponding hormone changes:
The Late Reproductive Stage
- Estrogen and FSH levels become variable
- Menstrual cycles remain regular or become slightly irregular
Early Perimenopause
- Estrogen and FSH levels become increasingly variable
- Menstrual cycles become increasingly irregular
- Menopausal symptoms may begin to appear
Late Perimenopause
- Menstrual cycles are irregular
- The probability of menopausal symptoms increases
Menopause
- Estrogen and progesterone levels are low
- FSH and LH levels are high
- No menstrual periods occur for 12 months or more
- There is a strong possibility of menopausal symptoms
Other relevant hormones include inhibin B and anti-mullerian hormone . Both of these are indicators of how many eggs remain in the ovaries, and their levels decrease throughout perimenopause and menopause.
What Is Fsh And Why Is It Important
Follicle stimulating hormone does exactly what it says it stimulates the ovaries to produce follicles each cycle.
The start of your period marks the beginning of the next cycle. This signals to your brain that its time to prepare a new egg for ovulation. To do this, it sends FSH to your ovaries.
Think of FSH like the fuel your ovaries need to grow follicles, like how a car needs gas to run. FSH gives your ovaries the energy they need to start growing follicles and maturing eggs. Eventually, one follicle and egg will become the most mature this is the egg that will ovulate that cycle.
At this point, you may know that people with ovaries are born with all the eggs theyll ever have this is referred to as your ovarian reserve. As you age and cycle over and over again, the amount of eggs you have slowly decreases over time.
When the ovaries have lots of eggs left, they dont need as much FSH to help recruit follicles because they have so many options to choose from. However, as you age and ovulate each cycle, you have less and less eggs to choose from.
With less eggs to recruit and mature, the ovaries need a little extra help to prepare for ovulation. So, the brain sends more FSH to the ovary. This is why low FSH levels signal a high ovarian reserve and high FSH levels signal a low ovarian reserve.
Don’t Miss: How To Test My Hormone Levels
How Do I Manage Symptoms Of Postmenopause On My Own
Certain lifestyle or at-home changes can help you manage symptoms of postmenopause. Some of these include:
- Regular exercise, meditation and other relaxing activities can help with depression and other side effects of postmenopause.
- Eating a diet rich in phytoestrogens such as whole-grain cereals, flaxseed, chickpeas and legumes. Reducing caffeine and alcohol intake has also been shown to help.
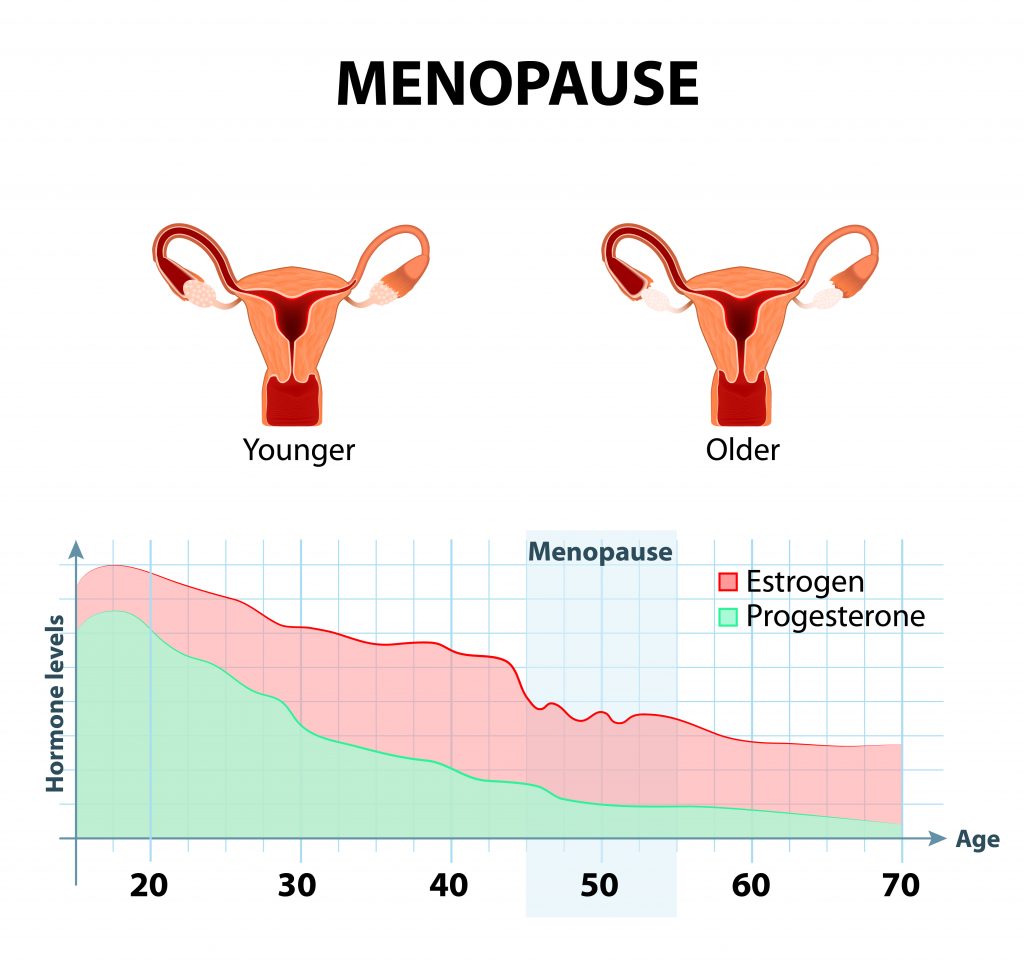
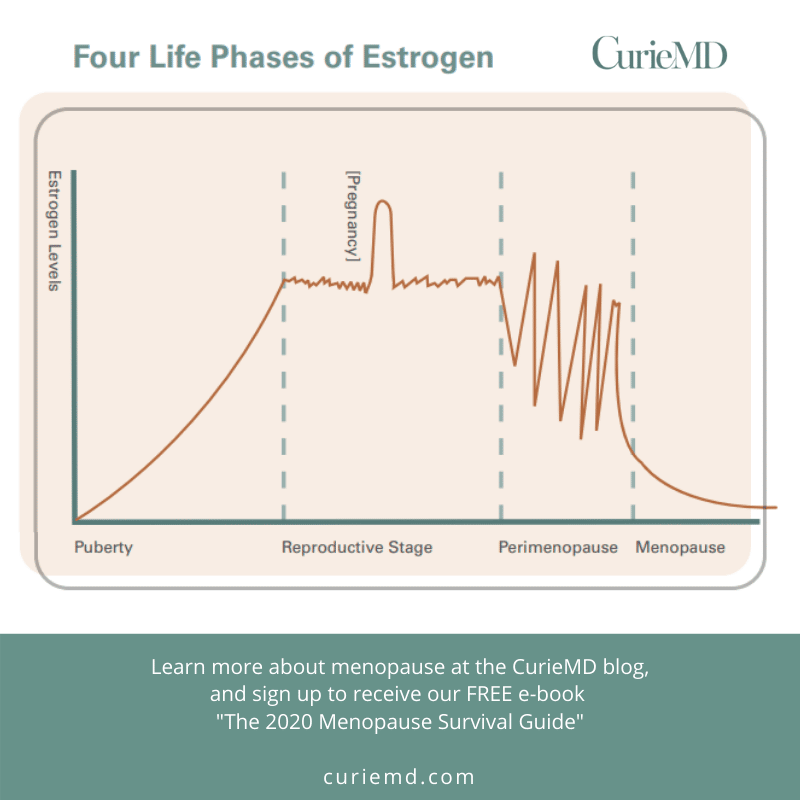
What Happens To Estrogen During Menopause
During women’s reproductive lives, estrogen levels are relatively consistent, guiding the menstrual cycle on a monthly basis alongside the hormone progesterone. Estrogen is produced largely by the ovaries with smaller amounts being produced by other organs.
Then, as women enter the menopausal transition, the ovaries wind down reproductive functions, and estrogen levels fluctuate unpredictably until postmenopause, which is when the hormone generally reaches consistently low levels.
As a matter of fact, after perimenopause ends, postmenopausal estrogen levels can be at 10 percent of what they are during premenopausal years.
As such, this hormonal imbalance brought on by estrogen’s fluctuations during perimenopause provokes various symptoms that are considered characteristic of this life transition.
Also Check: Are Testosterone Supplements Bad For You
What Is The Reason For Testing Hormone Levels
Dr. Rebecca: Good question. Hormone levels are helpful when we are tracking fertility and ovulation induction . Taken several times, they can give a very tentative window into where in the fertility transition a woman is.
But â and this is a big but â hormone levels are extremely variable throughout the cycle and even more irregular during the perimenopausal transition, so they become much less useful.
How To Understand Menopause Blood Test Results
As explained above, test results can be confusing to interpret, but the cut off points for FSH levels are relatively straightforward. A general guide is that a blood FSH level of > 30 IU/L suggests that the ovaries are slowing down, and can be taken as a potential indicator of menopause.
Can a blood test check what stage of menopause you have reached?
The simple answer is, not necessarily. However, a general rule is that FSH levels may be either normal or raised in perimenopause but will be raised at the postmenopausal stage.
Don’t Miss: How To Increase Your Hormones
How Do I Stay Healthy After Menopause
It is important to maintain a healthy lifestyle, especially as you age and your risk for certain medical conditions increases. Some ways for people in postmenopause to stay healthy include:
- Exercising regularly. Walking, doing yoga or strength training can help lower your risk for many medical conditions.
- Weight-bearing exercises can strengthen your bones and muscles.
- Eating a healthy diet. Foods like fruits, vegetables, lean meats and whole grains should make up the bulk of your diet. Avoid lots of salt or sugar and limit your consumption of alcohol.
A note from Cleveland Clinic
Going through menopause can be uncomfortable and present new challenges and health concerns. Speak with your healthcare provider about any symptoms you feel or questions you have. They can help make sure you are supported through this time and get the care you need.
Last reviewed by a Cleveland Clinic medical professional on 10/05/2021.
References
Symptoms Of An Estrogen Imbalance
The most common symptoms that can be brought on by an estrogen imbalance during menopause include:
- And other menopause symptoms
Keep in mind that while it is extremely common for an estrogen deficiency to provoke these symptoms, many women suffer from estrogen excess during menopause as well. Having high levels of estrogen in the body provokes similar symptoms as those of low estrogen.
The surest way to diagnose an estrogen imbalance in the body – whether high or low – is to see your doctor for appropriate testing.
Don’t Miss: How Do I Test My Estrogen Levels
Calcium And Vitamin D
A combination of calcium and vitamin D can reduce the risk of osteoporosis, the bone loss associated with menopause. The best sources are from calcium-rich and vitamin D-fortified foods.
Doctors are currently reconsidering the use of calcium and vitamin D supplements. The U.S. Preventive Services Task Force advises that healthy postmenopausal women don’t need to take these supplements. According to the USPSTF, taking daily low-dose amounts of vitamin D supplements , with or without calcium supplements , does not prevent fractures. For higher doses, the USPSTF says there is not enough evidence to make a recommendation. In addition to possible lack of benefit, these supplements are associated with certain risks, like kidney stones.
However, calcium and vitamin D are important nutrients. Supplements may be appropriate for certain people including those who do not get enough vitamin D through sunlight exposure and those who do not consume enough calcium in their diet. They are also helpful for people who have been diagnosed with osteoporosis. Talk with your doctor about whether or not you should take supplements.
The National Osteoporosis Foundation recommends:
Calcium
Vitamin D
Vitamin D is necessary for the absorption of calcium in the stomach and gastrointestinal tract and is the essential companion to calcium in maintaining strong bones.
This Program Changed My Life
I suffered constant fatigue, daily stomach pain, arthritis, insomnia, and bowel movements 7-8 times a day that precluded me from doing what I wanted. I was on several daily medications. This program changed my life. I have much more energy, especially in the morning, I sleep much better, no more stomach pain, I can walk 9 miles now, and dont need any medications. This program gave me the opportunity to enjoy life, instead of constant struggle.
Also Check: How To Lose Hormonal Belly
Will My Hot Flashes Stop After Menopause
Some people still experience hot flashes after menopause. Postmenopausal hot flashes are caused by decreased estrogen levels. It is not uncommon to experience a random hot flash for years after menopause. If your hot flashes are bothersome or intensify, speak with your healthcare provider to rule out other causes.
How Often Do I Need To See My Doctor After Menopause
You should still see your healthcare provider for routine gynecological care even though you aren’t menstruating. This includes Pap tests, pelvic exams, breast exams and mammograms. You should continue to schedule annual wellness appointments. Since you are at an increased risk for osteoporosis, providers usually recommend bone density screenings as well. Talk to your healthcare provider to determine how often you should make check-up appointments based on your health history.
You May Like: Can Taking Melatonin Cause Erectile Dysfunction
Recapitulating Human Female Reproductive Phases In Laboratory Animals
Estrogens actions are complex, and it is often challenging to systematically evaluate the biological underpinnings associated with estrogens actions in menopausal women. Therefore, multiple laboratories around the globe use rodent models that are invaluable tools for studying the impact of estrogen fluctuations on a variety of body systems including brain. Animal models provide researchers with opportunities to gain a fundamental understanding of the key elements underlying reproduction and aging processes, paving the way to explore novel pathways for intervention associated with known health risks. It is essential to keep in mind that some of the mechanisms associated with aging and the transition into a reproductively senescent state can differ when translating from one species to another.
Can I Test Myself For Menopause
You can use an at-home menopause test to measure your FSH level, which increases during menopause. However, these kits are not a surefire way of testing for menopause.
Nevertheless, if you use the tests, monitor your symptoms, and track your menstrual cycles, youll have a good overall understanding of your menopausal status.
A doctor can make a diagnosis of menopause depending on your symptoms, medical history, and a thorough health assessment.
Don’t Miss: What Hormones Makes You Happy
Other Drugs Used For Menopausal Symptoms
Despite its risks, hormone therapy appears to be the most effective treatment for hot flashes. There are, however, nonhormonal treatments for hot flashes and other menopausal symptoms.
Antidepressants
The antidepressants known as selective serotonin-reuptake inhibitors are sometimes used for managing mood changes and hot flashes. A low-dose formulation of paroxetine is approved to treat moderate-to-severe hot flashes associated with menopause. Other SSRIs and similar antidepressant medicines are used “off-label” and may have some benefit too. They include fluoxetine , sertraline , venlafaxine , desvenlafaxine , paroxetine , and escitalopram .
Gabapentin
Several small studies have suggested that gabapentin , a drug used for seizures and nerve pain, may relieve hot flashes. This drug is sometimes prescribed “off-label” for treating hot flash symptoms. However, in 2013 the FDA decided against approving gabapentin for this indication because the drug demonstrated only modest benefit. Gabapentin may cause:
Blood Tests For Hormone Levels In Menopause
For many women, working out whether or not youre in perimenopause or menopause can feel like a bit of a guessing game, especially if you are taking hormonal contraception, which can mask or cause one of the key signs of perimenopause and menopause your periods becoming irregular or absent. One option for women looking to understand where they are in their menopause journey is the use of a hormonal blood test, which can take a measure of your hormone levels to determine if you are in menopause. Hormonal blood tests work by measuring your hormone levels to work out whether or not you are menopausal. Menopause specialist, Dr Kate Burns, explains everything you need to know about blood tests, including how they work, when you should use them, how to read menopause blood test results, and how they can help.
Read Also: Go With The Flow Hormone Balance
General Recommendations For Ht
Current guidelines support the use of HT for the treatment of severe hot flashes that do not respond to non-hormonal therapies. General recommendations include:
- HT may be started in women who have recently entered menopause.
- HT should not be used in women who have started menopause many years ago.
- Women should not take HT if they have risks for stroke, heart disease, blood clots, and breast cancer.
- Currently, there is no consensus on how long HT should be used or at what age it should be discontinued. Treatment should be individualized for a woman’s specific health profile.
- HT should be used only for menopause symptom management, not for chronic disease prevention.
Initiating Therapy
Before starting HT, your doctor should give you a comprehensive physical exam and take your medical history to evaluate your risks for:
While taking HT, you should have regular mammograms and pelvic exams and Pap smears. Current guidelines recommend that if HT is needed, it should be initiated around the time of menopause. Studies indicate that the risk of serious side effects is lower for women who use HT while in their 50s. Women who start HT past the age of 60 appear to have a higher risk for side effects such as heart attack, stroke, blood clots, or breast cancer. HT should be used with care in this age group.
Discontinuing Therapy
Safety Concerns
Women who should not take hormone therapy include those with the following conditions: