Hormones And Your Pelvic Floor
As you may already know, the pelvic floor is essentially an area of muscles that stretch over your pelvic bone. Its role is to support your uterus, ovaries, bowel, and the infamous bladder just to name a few. During the menstrual cycle, pregnancy, perimenopause, and menopause, our pelvic floor changes A LOT. And guess whos partially responsible? Our hormones! Specifically estrogen, progesterone, and testosterone.
Medications For Prolapsed Bladder
Estrogen replacement therapy may be used for a prolapsed bladder to help the body strengthen the tissues in and around the vagina. Estrogen replacement therapy can’t be used by everyone . Womenâs bodies stop creating as much estrogen naturally after menopause, and the muscles of the vagina may weaken as a result. In mild cases of prolapsed bladder, estrogen may be prescribed in an attempt to reverse bladder prolapse symptoms, such as vaginal weakening and incontinence. For more severe degrees of prolapse, estrogen replacement therapy may be used along with other types of treatment.Estrogen can be administered orally as a pill or topically as a patch or cream. The cream has very little systemic absorption and has a potent effect locally where it is applied. Topical administration has less risk than the oral preparations. The application of estrogens to the anterior vagina and urethral area may be very helpful in alleviating urinary symptoms, such as urgency and frequency, even in the face of prolapsed bladder.
What Are The Next Steps
No matter the reason, frequent urination doesnt have to take over your life. Answers are only an appointment away.
Because once you know whats causing your frequent urination, youre that much closer to a peaceful nights sleep, uninterrupted jog around the lake or worry-free time doing whatever you like on your own terms.
Don’t Miss: Can Having Your Tubes Tied Cause Hormonal Imbalance
Is Frequent Urination A Sign Of Pregnancy
Women who are pregnant also tend to need to urinate more often. This is because the babies they are carrying cause the uterus to expand and put extra pressure on the bladder. Frequent urination during pregnancy is very common and typically not a cause for concern unless accompanied by other unexplained symptoms. Even after a baby is born, frequent urinate symptoms may continue. Women who have given birth vaginally in the past are at a greater risk of frequent urination. Giving birth in this way is known to make the pelvic floor weaker, and the pelvic floor is the body part that holds the bladder up and in place. This affects some women with children more than others.
Therefore, to conclude, frequent urination has numerous causes. Depending on how serious the cause is, fix your appointment with the doctor and take adequate care of yourself.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3749018/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695664/
Hope this article was of help to you! Please share your comments/queries/tips with us and help us create a world full of Happy, Healthy and Empowered Women!!
Menopause & Urinary Symptoms At A Glance:
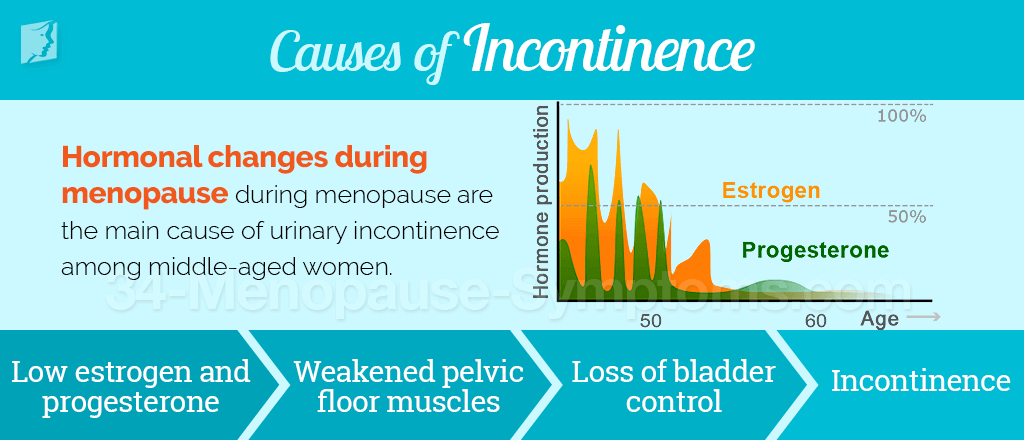
- Changes in a womans urinary function often accompany menopause. A primary cause is urogenital atrophy, which is the deterioration of the urinary tract and vagina.
- These urinary changes occur for two reasons: Menopause reduces the amount of the female hormone estrogen, and a lack of estrogen reduces the urinary tracts ability to control urination. Advanced age, which usually coincides with menopause, also has various debilitating effects on the pelvic area organs and tissues.
- Symptoms include the need to urinate more frequently, the inability to control urination , dryness and itching in the vagina, and increased urinary tract infections.
- Treatments vary and include dietary changes, strengthening exercises, topical estrogen for the vagina, and surgery.
Recommended Reading: Does Blue Cross Blue Shield Cover Low Testosterone
Weakened Pelvic Floor Muscles
Your pelvic floor muscles hold up many of the organs in your urinary system, including your bladder. If these muscles weaken, organs can slip slightly out of place and lead to more frequent urination. Vaginal childbirth is one way the pelvic floor muscles can become strained and start to lose their strength. Aging may also lead to pelvic floor muscle weakening.
Many times, it can be hard to tell if weakened pelvic floor muscles are causing your frequent urination. Your primary care doctor or OB-GYN can work with you to understand your symptoms, make treatment recommendations and connect you with a urogynecologist a doctor who specializes in diagnosing pelvic floor conditions if needed.
What Happens To The Pelvic Floor After A Hysterectomy
These are better known as the pelvic floor muscles. During a hysterectomy, there is an increased risk of damage to pelvic floor supportive structures which often results in bladder problems after hysterectomy. If during surgery they remove the ovaries, estrogen levels in the body will drop. Low estrogen levels weaken the tissues in the pelvic area.
Also Check: What Does Estrogen Cream Do
Will Hormone Replacement Help With Bladder Control
Many women complain of urine leakage with activity or with an uncontrollable urge .
Some women feel there is a worsening of the urinary incontinence around the time of the menses. Still others notice a worsening of incontinence symptoms with menopause, when estrogen levels drop to very low levels.
That estrogen plays a role in these symptoms is pretty certain, but exactly how it affects urinary incontinence is not clearly understood. Estrogen has a enhancing effect on the vaginal and urethral mucosa, and the pelvic floor muscles, rejuvenating the tissues and making them more elastic.
The most noticeable effects of estrogen on urinary tract symptoms occur when it is applied locally. This provides high levels that produce dramatic tissue effects, while limiting blood levels and exposure to other body areas such as uterus or breast.
Studies show an significant improvement in post menopausal women urinary symptoms with vaginal estrogen, but ironically an increase in the symptoms when estrogen is given orally. The latter is consistent with women complaining of a worsening of the incontinence with the profession of their cycle, although it is not known exactly why this seems to occur.
The take home message is that vaginal estrogen can significantly improve urinary incontinence symptoms in post menopausal women.
Oestrogens And Overactive Bladder
Estrogen has an important role in lower urinary tract function and dysfunction throughout adult life in women. Postmenopausal estrogen deficiency causes atrophic changes in the lower urinary tract and may be associated with urinary frequency, urgency, nocturia, and incontinence. The association of these changes with overactive bladder symptoms is unclear. Systemic and vaginal estrogens have been used for many years during and after menopause to manage urinary dysfunction despite the lack of adequate controlled trials confirming their efficacy. Data from large epidemiological studies have questioned the benefits of systemic estrogens for menopausal symptoms of incontinence and OAB. In the last decade, concerns regarding breast cancer and thromboembolic disease have been led to a marked reduction in the number of women seeking systemic hormone replacement therapy for menopausal symptoms.
The aim of this article was to review current evidence-based data on the effect of exogenous estrogen therapy on lower urinary tract function in menopausal and postmenopausal women, specifically those with symptoms of OAB. Evidence is reviewed on use of both systemic and vaginal estrogen therapy as well as combination therapy with antimuscarinic agents in this population.
Also Check: Can I Take Unisom And Melatonin
Estrogen Affects Your Bladder And Urethra
OAB due to menopause may be an effect of changing estrogen levels. Estrogen is the primary female sex hormone. Your ovaries produce most of your estrogen. Its essential to your sexual health and reproductive system. It also affects the health of other organs and tissues in your body, including your pelvic muscles and urinary tract.
Before menopause, a steady supply of estrogen helps preserve the strength and flexibility of your supportive pelvic and bladder tissues. During perimenopause and menopause, your estrogen levels drop dramatically. This can cause your tissues to weaken. Low estrogen levels may also contribute to muscular pressure around your urethra.
Changes in hormone levels may also increase the risk of urinary tract infections during perimenopause and menopause. UTIs may have similar symptoms as OAB. Talk to your doctor about any new changes to your urinary habits.
How Can I Treat Bladder Weakness
There are lots of medications that are available on prescription that are used to treated urinary incontinence. You will need to see your GP to discuss your symptoms so they can decide on the best method of treatment for you. Depending on your type of incontinence will depend on your treatment. Below are links to some of the treatment options available
Some of these treatments will need time to start working so if you need something more immediate to help you feel more comfortable then there are a wide range of feminine continence products available on the market now. Many of these have now been designed to be more discreet and can help to take away the embarrassment of urinary incontinence. You can find more information on the products available here.
Read Also: Can You Take Unisom With Melatonin
New Solutions For Menopause
Menopause is the time in a womans life when she stops having menstrual periods and can no longer get pregnant. It results from a decline in the production of the reproductive hormones estrogen and progesterone.
Although some women sail through menopause with few or no discomforts, shifting hormone levels cause some women to experience a variety of symptoms. These can include vaginal dryness, painful intercourse, chronic urinary tract infections , and changes in urinary habits.
If youre coping with chronic menopause-related UTIs, our providers at Womens Healthcare of Princeton can provide help that goes beyond just antibiotics. We offer a range of treatment options, including some new solutions that may surprise you.
How To Use Vaginal Estrogen Cream
If youre going through menopause and experiencing some of the discomforts of a hormonal imbalance, estrogen cream can help alleviate some of those symptoms.
Vaginal cream is designed to be used inside your vagina. It can be used right at the vaginal opening or inserted deeper inside.
To use vaginal estrogen cream, you need to be able to insert it into your vaginal canal. Follow these steps to get your applicator filled with the correct dosage:
- Wash your hands thoroughly with soap and warm water.
- Remove the cap from the tube of vaginal cream.
- Screw the nozzle part of the applicator onto the open end of the tube.
- Find the correct dosage. The applicator has markings on it that indicate how much cream will be inserted. Your doctor will give you the dosage amount they want you to use.
- Gently squeeze the tube so the cream fills the applicator to the required dosage mark.
- Unscrew the applicator from the tube, replace the cap on the tube, and set the tube aside.
Now that your applicator is filled and ready for use, you can insert it. You will be inserting the applicator tip into your vagina, so give yourself a few minutes of privacy and either wear easy-access clothing like a robe or remove your clothing. You will need to be in a room where you can lie down on your back.
How to insert the applicator:
Read Also: Can Cats Have Melatonin
Childbirth Trauma And Other Causes
Increased age is a common risk factor for pelvic floor disorders, including OAB and urinary incontinence. Some life phases can also affect your bladder. For example, pregnancy and childbirth can change the tone of your vagina, your pelvic floor muscles, and the ligaments that support your bladder.
Nerve damage from diseases and trauma can also cause mixed signals between the brain and the bladder. Medications, alcohol, and caffeine can also affect signals to the brain and cause the bladder to overflow.
What Causes Bladder Pain After Hysterectomy
The most common cause of pain after hysterectomy is vaginal or bladder prolapse. When they remove the uterus, the vagina is attached to supporting ligaments but these tissues can weaken over time. Roughly 10% of women will experience a vaginal vault prolapse in the years following their hysterectomy.
Read Also: Can Tubal Ligation Cause Early Menopause
How Is Low Estrogen Treated
Women who have low levels of estrogen may benefit from hormonal treatment. Hormonal treatment is the standard for low estrogen. There are non-hormonal options to help relieve symptoms. Non-hormonal options are preferred for women at high risk for breast cancer, blood clots, stroke, or liver disease.
Why Does Your Estrogen Level Matter
Estrogen is a hormone. Although present in the body in small amounts, hormones have big roles in maintaining your health.
Estrogen is commonly associated with the female body. Men also produce estrogen, but women produce it in higher levels.
The hormone estrogen:
- is responsible for the sexual development of girls when they reach puberty
- controls the growth of the uterine lining during the menstrual cycle and at the beginning of a pregnancy
- causes breast changes in teenagers and women who are pregnant
- is involved in bone and cholesterol metabolism
- regulates food intake, body weight, glucose metabolism, and insulin sensitivity
Girls who havent reached puberty and women approaching menopause are most likely to experience low estrogen. Still, women of all ages can develop low estrogen.
Common symptoms of low estrogen include:
You May Like: Tubal Ligation Cause Early Menopause
What Can I Expect If Ive Been Diagnosed With Vaginal Atrophy
You dont have to just live with vaginal atrophy. Even if youre in menopause or postmenopausal, that doesnt mean you should have to deal with UTIs, endure itching or burning, or painful sex. Treatment not only helps with symptoms, but it helps restore a healthy pH and bacterial balance back to your vagina.
What Is The Postmenopause
This is the stage of every womans life that follows the menopause, or her last menstrual period.
A woman is definitely postmenopausal when she has not had a period for at least a year. Most women in the UK go through the menopausal transition between the ages of 45 and 55, with the average age of the last menstrual period being about 52.
After the menopause the ovaries cease to produce the main female hormone, oestrogen, and its absence can produce a wide range of symptoms including the below In the long-term lack of oestrogen may predispose many women to:
- Osteoporosis.
- Night sweats
- Emotional changes
Many women also experience urogenital problems in the years after the menopause. Urogenital problems include the following:
- Urogenital atrophy Vaginal dryness
- Pelvic floor changes and prolapse For more information on prolapse, please visit our main Prolapse Section
- Lower urinary tract symptoms As they get older many women may find they have problems with their urinary tract . Some women may experience OAB leading to problems with urinary urgency. If you would like more information on bladder problems, please visit our main Bladder Problems section
- Recurrent urinary tract infections Commonly called cystitis, this is another form of a waterworks problem. A common symptom of cystitis is a burning pain when passing urine
Also Check: Does Blue Cross Blue Shield Cover Testosterone Therapy
What Else Can Cause Leakage
Menopause isnt always the reason why your bladder is acting up. Your muscles may have naturally weakened due to age. Or you might have had injuries as a result of giving birth to a child, or several children.
Condition like diabetes or multiple sclerosis can cause nerve damage, which in turn can also cause bladder problems.
Think about any medicines you take, too. Some antidepressants and pain meds can keep your bladder from emptying. Your doctor may be able to change your dose or prescription.
Continued
Low Estrogen May Contribute To Incontinence In Women
Significantly lower levels of oestrogen in peri-menopausal and post-menopausal women could increase their risk of stress urinary incontinence, according to Austrian researchers. They noted that sex steroid levels changed markedly during menopause, and oestrogen deficiency after menopause caused changes within the urogenital tract. Their study included 47 women with stress urinary incontinence who were matched with 47 controls. The findings suggested that low levels of circulating sex steroids might have a negative impact on the function of the lower urinary tract and on mechanisms involved with continence. Read more.
Nursing Times, June 8, 2017
Recommended Reading: Does Kaiser Cover Hormone Replacement Therapy
Menopause And Your Urinary Tract
It has been debated whether the changes in a woman’s urinary tract with age are due to menopause and the lack of estrogen, or instead related to the aging process alone. We do know, however, that the bladder is loaded with estrogen receptors, so the reduction of estrogen that happens in menopause probably doesn’t help.
With age, the bladder begins to lose both its volume and its elasticity, and it’s normal to have to go to the bathroom more frequently. As the bacteria concentration in your genital region increases your urethra may thin, allowing bacteria easier access to your bladder. For these reasons, urinary tract infections are more common as women age. This risk begins to increase within four or five years of your final menstrual period.
The bladder also begins to thin, leaving women more susceptible to incontinence, particularly if certain chronic illnesses or recurrent urinary tract infections are also present.
The pelvic muscles weaken as you age. You may find that exercise, coughing, laughing, lifting heavy objects, or performing any other movement that puts pressure on the bladder can cause small amounts of urine to leak. Lack of regular physical exercise may also contribute to this condition.
The Pattern Of Incontinence Is Often Mixed
Symptoms of overactive bladder include frequency and nocturia . Some women also feel they need to pass urine, having only just done so due to over activity of the bladder muscle.
Recurrent urinary tract infections
UTIs can affect women of all ages, but this problem increases with age as a result of estrogen deficiency.
Management of urinary problems
Local estrogen
Local estrogen replacement therapy has been shown to alleviate urgency, urge incontinence, frequency, nocturia, dysuria and also to reduce urine infections.
Genuine Stress Incontinence would not appear to be helped by estrogen alone, but it does seem to improve the action of other treatments currently used.
The newer treatments including Ospemifene, DHEA and laser therapy may all have a beneficial effect on bladder problems.
Pelvic floor exercises
These can strengthen the pelvic floor reducing the risk of uterovaginal prolapse. Many women have learnt these techniques from childbirth, but it is well worth revisiting them.
Pelvic-floor physiotherapists are specialists in this field and are able to fully assess and monitor a womans pelvic floor function and teach appropriate techniques to strengthen it and retrain the bladder. They often use devices to help women perform appropriate exercises, such as weighted vaginal cones, or vaginal trainers. Your practice nurse or GP should be able to refer you to a specialist pelvic floor physiotherapist.
Surgery
Recommended Reading: Does Tubal Ligation Cause Early Menopause