What Are The Side Effects Of Hormone Therapy
The side effects of hormone therapy depend largely on the specific drug or the type of treatment . The benefits and harms of taking hormone therapy should be carefully weighed for each person. A common switching strategy used for adjuvant therapy, in which patients take tamoxifen for 2 or 3 years, followed by an aromatase inhibitor for 2 or 3 years, may yield the best balance of benefits and harms of these two types of hormone therapy .
Hot flashes, night sweats, and vaginal dryness are common side effects of all hormone therapies. Hormone therapy also may disrupt the menstrual cycle in premenopausal women.
Less common but serious side effects of hormone therapy drugs are listed below.
Tamoxifen
- breathing problems, including painful breathing, shortness of breath, and cough
- loss of appetite
How Does The Brca1 Or Brca2 Gene Mutation Affect My Risk Of Breast Cancer Recurrence
Women with a BRCA1 or BRCA2 gene mutation and who have already been diagnosed with breast cancer, have a higher-than-average chance of new primary breast cancers than those without this genetic mutation. The chance of local or distant recurrence depends on the type and stage of the original breast cancer, and is no different from a non-BRCA-mutated breast cancer.
For women with a BRCA1 or BRCA2 gene mutation, the chance of a contralateral breast cancer, or cancer in the opposite breast to the original cancer, 10 years after diagnosis of the first cancer is about 10-30 percent compared to about 5-10 percent for women diagnosed with breast cancer who do not have a BRCA1 or BRCA2 gene mutation.
Women who have a BRCA1 or BRCA2 gene mutation and have received a breast cancer diagnosis, should talk to their treatment team about their options to reduce the risk of breast cancer recurrence.
How Common Is Breast Cancer Recurrence
Most local recurrences of breast cancer occur within five years of a lumpectomy. You can lower your risk by getting radiation therapy afterward. You have a 3% to 15% chance of breast cancer recurrence within 10 years with this combined treatment. Based on genetic testing, your provider may recommend additional treatments to further reduce your risk.
Recurrence rates for people who have mastectomies vary:
- There is a 6% chance of cancer returning within five years if the healthcare providers didnt find cancer in axillary lymph nodes during the original surgery.
- There is a one in four chance of cancer recurrence if axillary lymph nodes are cancerous. This risk drops to 6% if you get radiation therapy after the mastectomy.
Don’t Miss: When Can Kids Take Melatonin
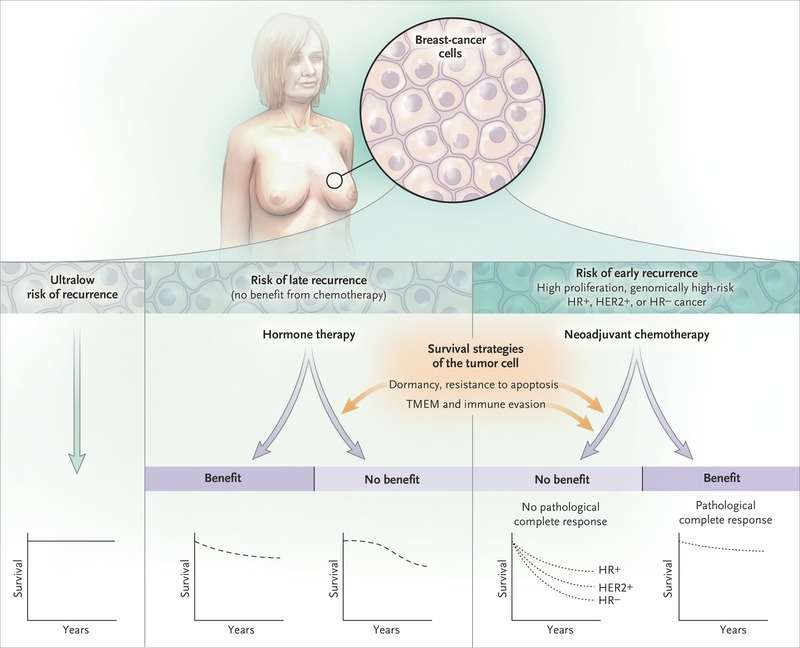
Early Recurrence Vs Late Recurrence
A recurrence of breast cancer at any time can be devastating. While 6% to 10% of breast tumors are diagnosed when the disease is already metastatic , 90% to 94% of metastatic breast cancers represent a distant recurrence of previous early-stage breast cancer .
Since distant metastases are responsible for around 90% of breast cancer deaths, finding ways to reduce the risk of recurrence is critical in improving the survival rate from the disease. Overall, it’s estimated that around 30% of breast cancers will recur at distant sites.
Study Selection And Data Synthesis
Two systematic searches of published literature were conducted on July 24, 2019 to identify eligible randomized controlled trials and observational or real-world evidence studies reporting any recurrence outcomes for adult patients with HR+/HER2- early BC receiving adjuvant ETs. Ovid MEDLINE®, MEDLINE® In-Process, Embase, and Evidence-Based Medicine Reviews were searched, restricting to articles published in the prior 15 years to reflect contemporary clinical practice, including the widespread approval for the most common AIs . The literature searches were conducted by an information specialist and peer-reviewed using the Peer Review of Electronic Search Strategies Guideline . Recent scientific congresses and relevant systematic reviews or meta-analysis articles were also reviewed. Citation titles and abstracts identified in the literature searches were screened for relevance then further evaluated in full-text form based on the same selection criteria. Literature searches, study selection, data extraction, and quality assessments were performed by duplicate independent reviewers , according to the Preferred Reporting Items for Systematic Review and Meta-Analysis statement. The review protocol was registered with the International Prospective Register of Systematic Reviews . The full search strategy, eligibility criteria, and list of excluded articles are available in the Supplementary.
Don’t Miss: Do Prenatal Vitamins Have Hormones
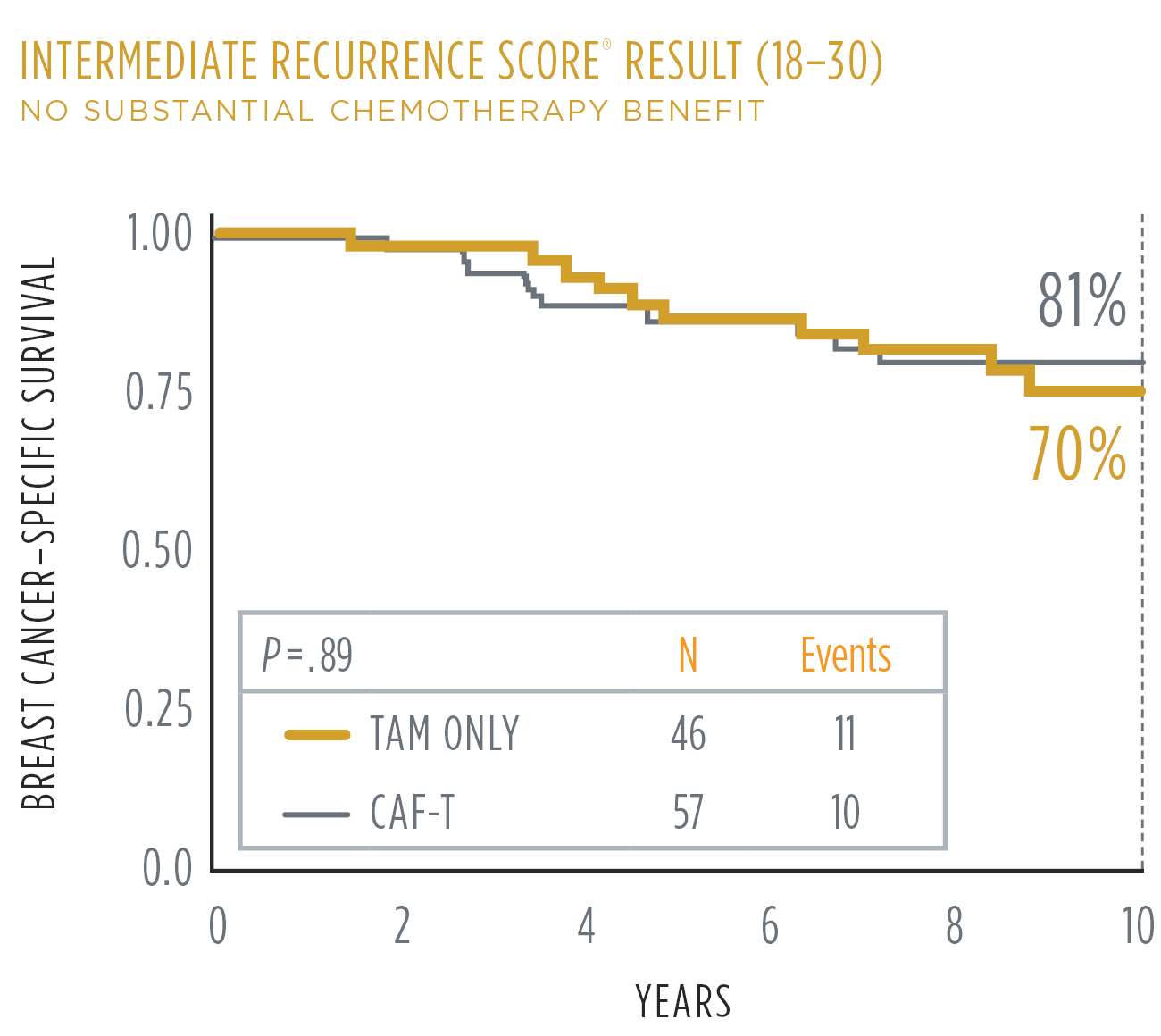
Current Understanding Of The Problem Of Late Recurrence
Earlier diagnosis of BC as a result of screening, coupled with the use of more effective systemic adjuvant therapy to prevent recurrences, has significantly improved clinical BC outcomes, particularly during the first 5 to 10years after diagnosis. Adjuvant chemotherapy and anti-HER2directed therapy substantially reduce the risk of recurrence, with the greatest risk reduction noted within the first 5years. Adjuvant endocrine treatment also reduces recurrence risk in patients with ER+ BC, with benefits observed within the first 5years and also after completing a 5-year course due to carryover effect associated with tamoxifen in particular.
In the workshop, we defined late recurrence as that occurring more than 5years after diagnosis and focused our deliberations on distant recurrence as opposed to local-regional recurrence or new ipsilateral or contralateral primary occurrences. Although the annual risk of distant recurrence is higher in the first 5years of follow-up and is decreased by adjuvant chemotherapy and ET, as many as one-half of the life-threatening BC recurrences and deaths in patients with ER+ HER2 BC take place in the succeeding 15 or more years, often after completion of adjuvant hormonal therapy . There is an urgent, unmet need to identify factors beyond standard clinical and pathologic features that affect the risk of recurrence and inform treatment decisions in individual patients.
Reduced Risk Of Distant Metastatic Disease
Based on the previous clinical trial STO-5, which was conducted between 1990 and 1997, researchers at Karolinska Institutet have now investigated the long-term treatment benefit of hormonal treatment in 584 premenopausal women with hormone-driven estrogen receptor-positive breast cancer. The study also includes a control group that had not received any hormonal treatment.
We could see that after 20 years, the risk of developing distant metastatic disease, i.e. spreading to other organs, had decreased among women who had received hormonal treatment with the drugs tamoxifen or goserelin or a combination of both, compared to those who had not received any hormonal treatment, says the study’s first author Annelie Johansson, postdoctoral fellow at the Department of Oncology-Pathology, Karolinska Institutet.
Recommended Reading: How To Lower Estrogen Dominance
Impact Of Late Recurrence
The impact of late distant recurrence cannot be stressed enough. Once breast cancer is metastatic, it is no longer curable. While there are some long term survivors with stage 4 breast cancer , the average life expectancy is currently only around three years.
Reducing Risk Of Recurrence
There are a number of myths regarding what may reduce the risk of breast cancer recurrence, as well as evidence-based information that is easily overlooked. We will look at measures that may reduce your risk based on credible studies, as well as practices that are unclear that you may wish to discuss with your oncologist.
In some cases, though the benefit on recurrence risk is still not clear, your quality of life may be improved. And living well with cancer is as important as extending your life with cancer.
Before talking about measures that may help lower recurrence risk, it’s important to not add to the stigma of the disease. Some people do absolutely everything right and their breast cancer recurs anyway. Similarly, some people eat poorly, smoke, and drink heavily and their cancer never recurs. While you may be able to decrease your risk of recurrence to a degree, dealing with breast cancer is dealing with a mutated clone of cells that doesn’t think or follow the rules.
For those who have a recurrence, it doesn’t mean they have done anything wrong. It simply means cancer is being cancer.
Recommended Reading: What Supplements Are Good For Hormonal Acne
Risk Of Late Recurrence Is Underestimated
A survey led by the Canadian Breast Cancer Network found that women often underestimate their risk of late recurrence. In the survey, only 10% were aware of the risk of recurrence after five years of tamoxifen therapy, and 40% felt that they were cured after hitting the five-year mark.
Many breast cancer survivors underestimate their risk of late recurrence.
Address Any Sleep Problems You Have
According to a 2017 study, cisgender women who experience regular sleep difficulties, as well as those who have a prolonged sleep duration have a greater all-cause as well as breast cancer mortality rate.
There are a number of different types of sleep disorders, and these, in turn, are often addressed in different ways. For starters, practicing good sleep hygiene habits can sometimes resolve minor sleep problems.
If problems persist, however, talking to a sleep expert may be in order. We often think of sleep as inconsequential , but given the link between sleep disturbances and survival it might be considered as important as some of the treatments we use to battle the disease.
Read Also: Hormones For Transgender Female To Male
Possible To Predict Future Risk
The researchers have, in recent years, also analysed the patients’ tumours from the previous STO-5 study using modern technology. For example, they have investigated various breast cancer markers, such as the estrogen receptor and the progesterone receptor, and tumour gene expression using a gene-risk signature.
The signature measures the activity of 70 different genes, which are calculated into risk points. This makes it possible to predict the future development of the tumour cells at an early stage and thus categorise the patients into low and high genomic risk, respectively.
The tumours in patients with high genomic risk often have a higher cancer growth rate. Therefore, these patients have an earlier risk of relapse where a more aggressive treatment is needed, such as with goserelin, which quickly and effectively reduces estrogen levels. On the other hand, patients with a less aggressive disease may have a long-term risk of recurrence. In these cases, tamoxifen appears to offer a better protection, says Annelie Johansson.
Although the study is relatively small, it highlights the importance of individualised treatments against hormone-driven breast cancer. For some patients, a more aggressive treatment may be necessary for survival, whilst a milder treatment may be sufficient for others, reducing side effects and providing a better quality of life. However, further studies are needed before major changes in treatment recommendations can be implemented.
Locally Advanced Breast Cancer
If breast cancer has spread to the chest wall or skin of the breast, or the lymph nodes around the chest, neck and under the breast bone, but has not spread to other areas of the body, its called locally advanced breast cancer. Sometimes breast cancer is locally advanced when it is first diagnosed.
People who have locally advanced breast cancer are thought to have an increased risk of cancer cells spreading to other areas of the body, compared to those with stage 1 or 2 breast cancers.
Read Also: How To Keep My Hormones Balanced
Maintain A Healthy Body Weight
Maintaining a healthy weight appears to lower the risk of breast cancer recurrence. If you’ve been frustrated in attempts to lose weight in the past, it may be encouraging to know that some other practices on this list are associated with weight loss, not just exercise, but intermittent fasting, and even upping the fiber in your diet to improve the diversity of the bacteria in your gut.
The Myth And Stigma Of The 5
Many people still believe that breast cancer, even hormone-positive disease, is essentially cured after five years this can lead to misunderstandings in families. Loved ones who don’t understand late recurrence may downplay your feelings, or criticize you when you think “brain tumor” each time you get a headache.
Until information on late recurrence becomes more widely known, and even though it’s frustrating, you may need to educate loved ones about the risk, and why you should be concerned when you develop new or unexplained symptoms.
You May Like: How To Treat Hormonal Acne In Your 30’s
Histopathological Evaluation Of Til Density
TIL density was evaluated pathologically using biopsy specimens. The pathological diagnosis and examination were jointly performed by two breast pathologists. The definition and evaluation method for TILs followed the International TILs Working Group 2014 . Specifically, the density of infiltrating lymphocytes was averaged on full sections, at least five fields, of the tumor stroma. The results were divided into four groups according to previous reports .
Fig. 1
Histopathologic evaluation of the tumor-infiltrating lymphocytes density was performed on hematoxylin and eosin-stained tumor section. The density of them was averaged on full sections, at least five fields, of the tumor stroma. The results were divided into four groups ,> 1050% ,10% , and absent , respectively)
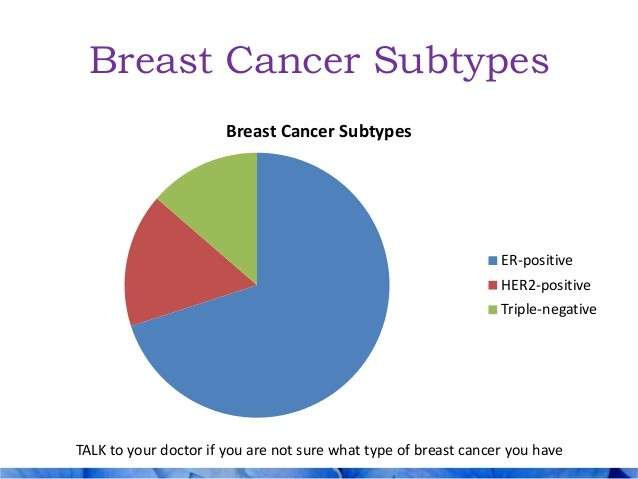
What Types Of Hormone Therapy Are Used For Breast Cancer
Several strategies are used to treat hormone-sensitive breast cancer:
Blocking ovarian function: Because the ovaries are the main source of estrogen in premenopausal women, estrogen levels in these women can be reduced by eliminating or suppressing ovarian function. Blocking ovarian function is called ovarian ablation.
Ovarian ablation can be done surgically in an operation to remove the ovaries or by treatment with radiation. This type of ovarian ablation is usually permanent.
Alternatively, ovarian function can be suppressed temporarily by treatment with drugs called gonadotropin-releasing hormone agonists, which are also known as luteinizing hormone-releasing hormone agonists. By mimicking GnRH, these medicines interfere with signals that stimulate the ovaries to produce estrogen.
Estrogen and progesterone production in premenopausal women. Drawing shows that in premenopausal women, estrogen and progesterone production by the ovaries is regulated by luteinizing hormone and luteinizing hormone-releasing hormone . The hypothalamus releases LHRH, which then causes the pituitary gland to make and secrete LH and follicle-stimulating hormone . LH and FSH cause the ovaries to make estrogen and progesterone, which act on the endometrium .
Examples of ovarian suppression drugs are goserelin and leuprolide .
Blocking estrogens effects: Several types of drugs interfere with estrogens ability to stimulate the growth of breast cancer cells:
Also Check: Hormonal Acne And Dry Skin
What This Means For You
If youâve been diagnosed with early-stage breast cancer, your doctor may recommend treatments after surgery to reduce your risk of recurrence.
If you were diagnosed with hormone receptor-positive, early-stage breast cancer, itâs likely that your doctor will recommend you take some type of hormonal therapy medicine â either tamoxifen or an aromatase inhibitor depending on your menopausal status â for five to 10 years after surgery.
Chemotherapy after surgery is usually completed in three to six months. If youâre also receiving a targeted therapy, such as Herceptin , with chemotherapy, you may continue to receive the targeted therapy for up to a year after completing chemotherapy.
Radiation therapy after surgery can be completed in one to seven weeks.
So, hormonal therapy after surgery takes the longest to complete. Hormonal therapy medicines also can cause troubling side effects, such as hot flashes, night sweats, and joint pain. Less common but more severe side effects include heart problems and blood clots.
Research has shown that about 25% of women who are prescribed hormonal therapy to reduce the risk of recurrence after surgery either donât start taking the medicine or stop taking it early, in many cases because of side effects.
Learn more about Staying on Track With Treatment. You can read about why itâs so important to stick to your treatment plan, as well as ways to manage side effects after radiation, chemotherapy, and hormonal therapy.
What Factors Contribute To The Risk Of Breast Cancer Recurrence
Whilst it is never completely certain that breast cancer has been cured, there are many treatments available that reduce the risk of recurrence. There are a number of risk factors that can contribute to a breast cancer recurrence.
Your age at first diagnosis Younger women, particularly those who had their first diagnosis under the age of 35, have a greater risk of recurrence. This is because those diagnosed at a young age are more likely to have aggressive features in their breast cancer. Additionally women diagnosed with breast cancer before menopause have a greater risk of recurrence.
Tumour size Women who have a larger breast tumour have a greater risk of recurrence.
Lifestyle factors Lifestyle factors can influence the risk of recurrence. Excess weight is associated with a higher risk of postmenopausal breast cancer and is also associated with a higher risk of breast cancer recurrence and death. Smoking has also been shown to increase the risk of recurrence. Women who exercise regularly appear to have a lower rate of breast cancer recurrence.
Lymph node involvement If cancer is found in lymph nodes at the time of the original breast cancer diagnosis, there is an increased risk of breast cancer recurrence. This is the strongest prognostic factor, and the more nodes involved, the higher the risk of recurrence.
Read Also: Where To Buy Testosterone Gel
Who Is At Risk Of Breast Cancer Recurrence
Everyone who has received a breast cancer diagnosis is at risk of recurrence, however the risk differs markedly depending on a number of factors listed below. Some breast cancers, when diagnosed very early when small and without lymph node involvement, have an excellent prognosis and are very unlikely to recur. On the contrary, larger cancers, with lymph node involvement or with a more invasive behaviour, are unfortunately at a higher risk of recurrence.
Risk Factors For Overall Recurrence
There are several risk factors that raise the risk of recurrence overall . These include:
- Tumor size: Larger tumors are more likely to recur than smaller ones both early and late.
- Positive lymph nodes: Tumors that have spread to lymph nodes are more likely to recur at any time than those that have not.
- Age at diagnosis: Breast cancer recurrence is more common in younger people.
- Treatments received and response to treatments: Both chemotherapy and hormonal therapy reduce the risk of recurrence in the first five years.
- Tumor grade: More aggressive tumors are more likely to recur than less aggressive tumors , especially in the first five years.
There are also factors that do not appear to affect the risk of recurrence. Recurrence rates are the same for women who have a mastectomy or lumpectomy with radiation and are also the same for women who have a single vs. double mastectomy.
Also Check: What Can I Take To Boost My Testosterone