Drugs That Block Estrogen
Some drugs work by blocking estrogen from causing cancer cells to grow.
Tamoxifen is a drug that prevents estrogen from telling cancer cells to grow. It has a number of benefits:
- Taking Tamoxifen for 5 years after breast cancer surgery cuts the chance of cancer coming back by half. Some studies show that taking it for 10 years may work even better.
- It reduces the risk that cancer will grow in the other breast.
- It slows the growth and shrinks cancer that has spread.
- It reduces the risk of getting cancer in women who are at high risk.
Other drugs that work in a similar way are used to treat advanced cancer that has spread:
- Toremifene
- Fulvestrant
Study Selection And Data Synthesis
Two systematic searches of published literature were conducted on July 24, 2019 to identify eligible randomized controlled trials and observational or real-world evidence studies reporting any recurrence outcomes for adult patients with HR+/HER2- early BC receiving adjuvant ETs. Ovid MEDLINE®, MEDLINE® In-Process, Embase, and Evidence-Based Medicine Reviews were searched, restricting to articles published in the prior 15 years to reflect contemporary clinical practice, including the widespread approval for the most common AIs . The literature searches were conducted by an information specialist and peer-reviewed using the Peer Review of Electronic Search Strategies Guideline . Recent scientific congresses and relevant systematic reviews or meta-analysis articles were also reviewed. Citation titles and abstracts identified in the literature searches were screened for relevance then further evaluated in full-text form based on the same selection criteria. Literature searches, study selection, data extraction, and quality assessments were performed by duplicate independent reviewers , according to the Preferred Reporting Items for Systematic Review and Meta-Analysis statement. The review protocol was registered with the International Prospective Register of Systematic Reviews . The full search strategy, eligibility criteria, and list of excluded articles are available in the Supplementary.
Dont Miss: Do Prenatal Vitamins Have Hormones
Having Hormonal Therapy For Breast Cancer
Hormonal therapy drugs reduce the risk of breast cancer coming back. It is important to take it for as long as you have been prescribed it for. Try to make taking it part of your daily routine so it becomes a habit.
Most women cope well with the side effects of hormonal therapy. They may be more of a problem in the first few months, but usually get better over time. If the side effects do not improve or are difficult to cope with, talk to your specialist nurse or cancer doctor. They can prescribe drugs to help and suggest ways of coping.
If you are still having problems after this, then your cancer doctor may suggest changing to a different type of hormonal therapy.
Also Check: Can You Get Addicted To Melatonin
What This Means For You
If youâve been diagnosed with early-stage breast cancer, your doctor may recommend treatments after surgery to reduce your risk of recurrence.
If you were diagnosed with hormone receptor-positive, early-stage breast cancer, itâs likely that your doctor will recommend you take some type of hormonal therapy medicine â either tamoxifen or an aromatase inhibitor depending on your menopausal status â for five to 10 years after surgery.
Chemotherapy after surgery is usually completed in three to six months. If youâre also receiving a targeted therapy, such as Herceptin , with chemotherapy, you may continue to receive the targeted therapy for up to a year after completing chemotherapy.
Radiation therapy after surgery can be completed in one to seven weeks.
So, hormonal therapy after surgery takes the longest to complete. Hormonal therapy medicines also can cause troubling side effects, such as hot flashes, night sweats, and joint pain. Less common but more severe side effects include heart problems and blood clots.
Research has shown that about 25% of women who are prescribed hormonal therapy to reduce the risk of recurrence after surgery either donât start taking the medicine or stop taking it early, in many cases because of side effects.
Learn more about Staying on Track With Treatment. You can read about why itâs so important to stick to your treatment plan, as well as ways to manage side effects after radiation, chemotherapy, and hormonal therapy.
Surgery To Stop The Ovaries From Working
This is also a type of ovarian ablation. You might choose to have an operation to remove your ovaries instead of having drug treatment to stop them working. You have this operation as keyhole surgery. It is called laparoscopic oophorectomy and you have it under general anaesthetic . You usually stay in hospital overnight.
The surgeon makes a number of small cuts into your tummy . They put a long bendy tube called a laparoscope into one of the cuts. The laparoscope connects to a video screen.
The surgeon puts small instruments through the other cuts to carry out the operation and remove the ovaries. They close the cuts with stitches and cover them with small dressings.
Removing your ovaries causes you to have a sudden menopause. The symptoms include hot flushes, sweating and mood swings.
Also Check: What Supplements Are Good For Hormone Imbalance
If Cancer Has Come Back Or Spread
Hormone therapy can be used to treat breast cancer that has come back or that has spread to another part of the body .
Its given either alone or with other treatments, depending on what treatments you had before.
If your breast cancer came back during or after treatment with hormone therapy, you may be offered a different type of hormone therapy.
What Factors Contribute To The Risk Of Breast Cancer Recurrence
Whilst it is never completely certain that breast cancer has been cured, there are many treatments available that reduce the risk of recurrence. There are a number of risk factors that can contribute to a breast cancer recurrence.
Your age at first diagnosis Younger women, particularly those who had their first diagnosis under the age of 35, have a greater risk of recurrence. This is because those diagnosed at a young age are more likely to have aggressive features in their breast cancer. Additionally women diagnosed with breast cancer before menopause have a greater risk of recurrence.
Tumour size Women who have a larger breast tumour have a greater risk of recurrence.
Lifestyle factors Lifestyle factors can influence the risk of recurrence. Excess weight is associated with a higher risk of postmenopausal breast cancer and is also associated with a higher risk of breast cancer recurrence and death. Smoking has also been shown to increase the risk of recurrence. Women who exercise regularly appear to have a lower rate of breast cancer recurrence.
Lymph node involvement If cancer is found in lymph nodes at the time of the original breast cancer diagnosis, there is an increased risk of breast cancer recurrence. This is the strongest prognostic factor, and the more nodes involved, the higher the risk of recurrence.
Read Also: Where To Buy Testosterone Gel
You May Like: Does Hyaluronic Acid Increase Estrogen
Hormones And Breast Cancer
The hormones estrogen and progesterone make some breast cancers grow. They are called hormone-sensitive breast cancers. Most breast cancers are sensitive to hormones.
Estrogen and progesterone are produced in the ovaries and other tissues such as fat and skin. After menopause, the ovaries stop producing these hormones. But the body continues to make a small amount.
Hormone therapy only works on hormone-sensitive cancers. To see if hormone therapy may work, doctors test a sample of the tumor that has been removed during surgery to see if the cancer might be sensitive to hormones.
Hormone therapy can work in two ways:
What Are Hormones And Hormone Receptors
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and in men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
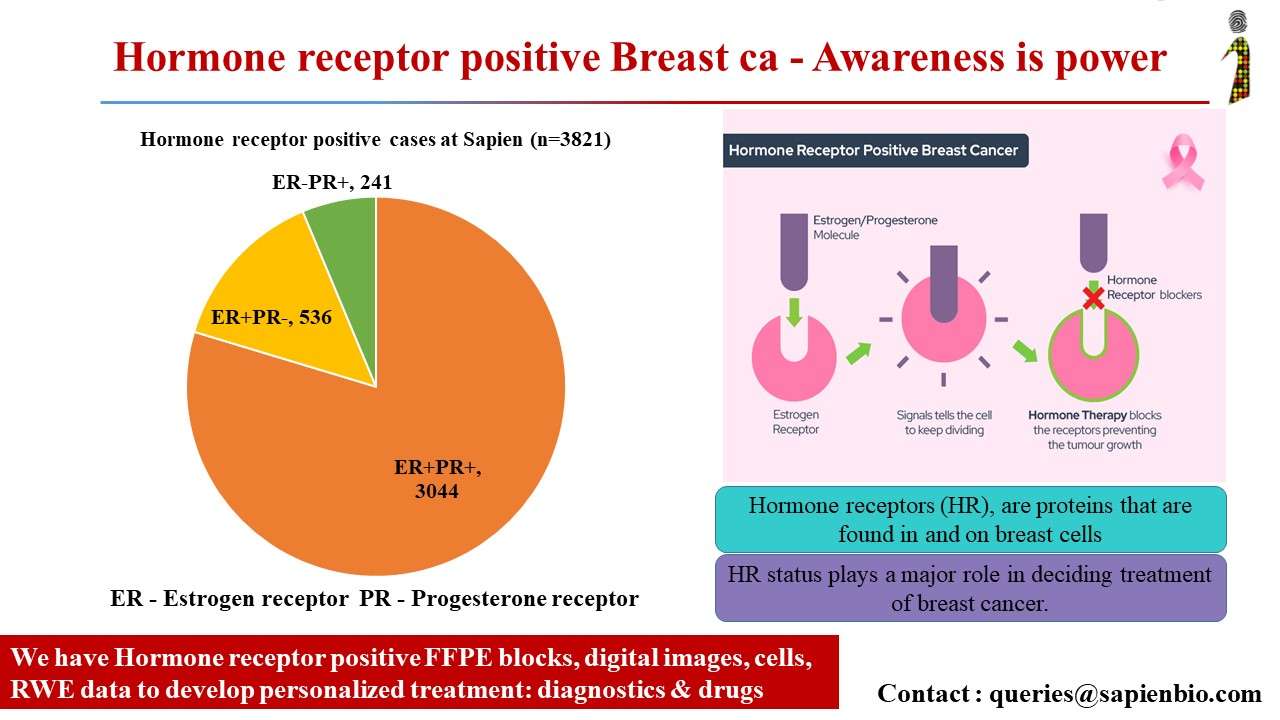
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive breast cancers. Hormone-sensitive breast cancer cells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
Breast cancers that lack ERs are called ER negative, and if they lack both ER and PR they may be called HR negative.
Approximately 67%80% of breast cancers in women are ER positive . Approximately 90% of breast cancers in men are ER positive and approximately 80% are PR positive .
Also Check: What Are The Side Effects Of Low Estrogen
Expert Review And References
- Bursein HJ, Harris JR, Morrow M. Malignant tumors of the breast. Devita, V. T., Jr., Lawrence, T. S., & Rosenberg, S. A. Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins 2008: 43.2: pp. 1606-54.
- Foxson SB, Lattimer JG & Felder B. Breast cancer. Yarbro, CH, Wujcki D, & Holmes Gobel B. . Cancer Nursing: Principles and Practice. 7th ed. Sudbury, MA: Jones and Bartlett 2011: 48: pp. 1091-1145.
- National Cancer Institute. Breast Cancer Treatment Health Professional Version. Bethesda, MD: National Cancer Institute 2010.
- Breast cancer. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. National Comprehensive Cancer Network 2010.
- Tripathy D, Eskenazi LB, Goodson, WH, et al. Breast. Ko, A. H., Dollinger, M., & Rosenbaum, E. Everyone’s Guide to Cancer Therapy: How Cancer is Diagnosed, Treated and Managed Day to Day. 5th ed. Kansas City: Andrews McMeel Publishing 2008: pp. 473-514.
Possible To Predict Future Risk
The researchers have, in recent years, also analysed the patients tumours from the previous STO-5 study using modern technology. For example, they have investigated various breast cancer markers, such as the estrogen receptor and the progesterone receptor, and tumour gene expression using a gene-risk signature.
The signature measures the activity of 70 different genes, which are calculated into risk points. This makes it possible to predict the future development of the tumour cells at an early stage and thus categorise the patients into low and high genomic risk, respectively.
The tumours in patients with high genomic risk often have a higher cancer growth rate. Therefore, these patients have an earlier risk of relapse where a more aggressive treatment is needed, such as with goserelin, which quickly and effectively reduces estrogen levels. On the other hand, patients with a less aggressive disease may have a long-term risk of recurrence. In these cases, tamoxifen appears to offer a better protection, says Annelie Johansson.
Although the study is relatively small, it highlights the importance of individualised treatments against hormone-driven breast cancer. For some patients, a more aggressive treatment may be necessary for survival, whilst a milder treatment may be sufficient for others, reducing side effects and providing a better quality of life. However, further studies are needed before major changes in treatment recommendations can be implemented.
Recommended Reading: How To Treat Adult Hormonal Acne
What Types Of Hormone Therapy Are Used For Breast Cancer
Several strategies are used to treat hormone-sensitive breast cancer:
Blocking ovarian function: Because the ovaries are the main source of estrogen in premenopausal women, estrogen levels in these women can be reduced by eliminating or suppressing ovarian function. Blocking ovarian function is called ovarian ablation.
Ovarian ablation can be done surgically in an operation to remove the ovaries or by treatment with radiation. This type of ovarian ablation is usually permanent.
Alternatively, ovarian function can be suppressed temporarily by treatment with drugs called gonadotropin-releasing hormone agonists, which are also known as luteinizing hormone-releasing hormone agonists. By mimicking GnRH, these medicines interfere with signals that stimulate the ovaries to produce estrogen.
Estrogen and progesterone production in premenopausal women. Drawing shows that in premenopausal women, estrogen and progesterone production by the ovaries is regulated by luteinizing hormone and luteinizing hormone-releasing hormone . The hypothalamus releases LHRH, which then causes the pituitary gland to make and secrete LH and follicle-stimulating hormone . LH and FSH cause the ovaries to make estrogen and progesterone, which act on the endometrium .
Examples of ovarian suppression drugs are goserelin and leuprolide .
Blocking estrogens effects: Several types of drugs interfere with estrogens ability to stimulate the growth of breast cancer cells:
Drugs That Lower Estrogen Levels
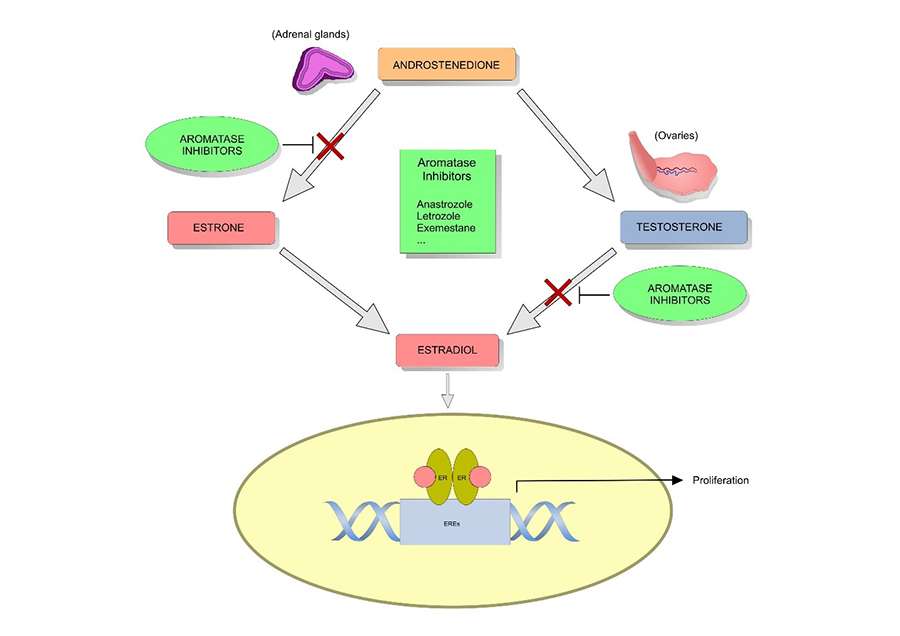
Some drugs, called aromatase inhibitors , stop the body from making estrogen in tissues such as fat and skin. But, these drugs do not work to make the ovaries stop making estrogen. For this reason, they are used mainly to lower estrogen levels in women who have been through menopause . Their ovaries no longer make estrogen.
Premenopausal women can take AIs if they are also taking drugs that stop their ovaries from making estrogen.
Aromatase inhibitors include:
- Exemestane
Recommended Reading: What Are Bioidentical Hormones Used For
Address Any Sleep Problems You Have
According to a 2017 study, cisgender women who experience regular sleep difficulties, as well as those who have a prolonged sleep duration have a greater all-cause as well as breast cancer mortality rate.
There are a number of different types of sleep disorders, and these, in turn, are often addressed in different ways. For starters, practicing good sleep hygiene habits can sometimes resolve minor sleep problems.
If problems persist, however, talking to a sleep expert may be in order. We often think of sleep as inconsequential , but given the link between sleep disturbances and survival it might be considered as important as some of the treatments we use to battle the disease.
Read Also: Hormones For Transgender Female To Male
How Can Hormones Affect The Growth Of Breast Cancer
Hormones like estrogen and progesterone are chemicals produced by glands in the body. Normally, these hormones help regulate body cycles, like menstruation. However, sometimes these same hormones can cause cancer to grow.
The pathologist will perform tests on the breast cancer cells to determine if they have receptors that feed on estrogen or progesterone, stimulating their growth. If the cancer cells have these receptors, your doctor may recommend hormone therapy drugs, such as blockers or inhibitors. Both types of drugs help to destroy cancer cells by cutting off their supply of hormones.
You May Like: How Much Does It Cost To Get Hormone Levels Checked
What Are Hormone Receptors
Breast cancers that are hormone receptor positive have receptors for the female hormones oestrogen and/or progesterone on the inside of the cancer cells.
In breast cancer cells that are hormone receptor positive, oestrogen and/or progesterone, which are naturally produced in the body, make the cancer grow. You can think of it as the receptor being the lock and oestrogen being the key. The oestrogen fits into the receptor and switches the cancer cell on, causing it to grow. Hormone therapy for breast cancer can starve cancer cells by upsetting this process.
Testing for hormone receptors is part of the routine pathology testing following surgery. Testing is done on a core biopsy sample if surgery is not planned.
Your doctor will be able to tell you if your breast cancer is hormone receptor positive or not. Most, but not all breast cancer is hormone receptor positive.
The hormonal therapies described in this brochure only work against breast cancers that are hormone receptor positive. Other treatments need to be used for cancers that are hormone receptor negative.
If Cancer Comes Back Or Has Spread
AIs, tamoxifen, and fulvestrant can be used to treat more advanced hormone-positive breast cancers, especially in post-menopausal women. They are often continued for as long as they are helpful. Pre-menopausal women might be offered tamoxifen alone or an AI in combination with an LHRH agonist for advanced disease.
Recommended Reading: Is There Natural Estrogen Replacement
Adjuvant Hormonal Therapy Treatment Time
For many years, women took hormonal therapy for five years after surgery for early-stage, hormone receptor-positive breast cancer. In most cases, the standard of care is five years of tamoxifen, or two to three years of tamoxifen followed by two to three years of an aromatase inhibitor, depending on menopausal status.
Recent research has found that in certain cases, taking tamoxifen for 10 years instead of five years after surgery lowered a womans risk of recurrence and improved survival.
In most cases, a post-menopausal woman diagnosed with early-stage, hormone receptor-positive breast cancer would take an aromatase inhibitor for five years after surgery to reduce the risk of recurrence. After that, if breast cancer had been found in the lymph nodes, called node-positive disease, a woman would take an aromatase inhibitor for an additional five years, for a total of 10 years of hormonal therapy treatment.
Doctors call taking hormonal therapy for 10 years after surgery extended adjuvant hormonal therapy.
Predicting Outcome In Er+ Patients
The current clinical questions include prospective validation of the Oncotype recurrence score to determine the benefit of chemotherapy in the intermediate risk groups which was not clear in the previously mentioned trials. Also needed is an analysis of recurrence score in the context of more contemporaneous chemotherapies such as taxanes, and endocrine therapies such as aromatase inhibitors. The National Cancer Institute sponsored, TAILORx trial has been designed to answer these questions. In this study, in which all major American cooperative groups participated, nearly 9000 patients were enrolled and accrual is complete. Importantly, patients with recurrence score of 1125 are randomized to receive endocrine therapy alone or chemotherapy followed by endocrine therapy. The primary objective is to assess noninferiority of endocrine therapy alone compared with the combination. An additional study is now evaluating the use of Oncotype in postmenopausal women with intermediate risk HRpositive, nodepositive breast cancer . Similarly, a large prospective evaluation of the MammaPrint assay is being evaluated primarily in Europe. This trial, entitled the MINDACT trial is being conducted by the European Organization for Research and Treatment of Cancer and the TRANSBIG research consortium.
You May Like: How Much Are Male To Female Hormones