How Does The Mirena Work
The Mirena IUD, like all hormonal IUDs, contains a synthetic hormone called Levonorgestrel, a progestin, that it slowly releases in your body over time. While progestin sounds like progesterone, it is not, nor does it behave like progesterone in your body.
Instead, the progestin released thins the lining of your uterus, the endometrium, so a fertilized egg would be unable to implant. This is one way in which women have lighter or absent periods while using a hormonal IUD.
It is also designed to stop ovulation by suppressing the production of two brain hormonesFollicle Stimulating Hormone and Luteinizing Hormone . FSH and LH work together to mature an egg and trigger ovulation. They are also responsible for signaling the rise and fall of your hormones. It also thickens cervical secretions, making it difficult for sperm to make it to the egg in the event ovulation does occur.
All About The Hormonal Iud
- – Dr Libby Weaver
The hormonal IUDcommonly known by the brand name Mirena®is a small, plastic T-shaped device that is inserted into the uterus. It is considered a long-acting form of contraception as it can remain in place for a number of years. It releases small amounts of a progestin hormone into the uterus. Progestins are synthetic substances that are similar to progesterone, but not identical. They mimic some of the effects of progesteronesuch as reducing bleedingbut they dont have all of the same actions and benefits that progesterone does.
Expulsionyour Uterus Kicks It Out
Expulsion occurs after an IUD is placed and is your uterus pushing the device out. Hormonal IUDs, like the Mirena, come with a 3-6 percent expulsion rate in the first year. Comparatively, the copper IUD is associated with a 3-10 percent risk of expulsion in the first year.
Who is at risk of IUD expulsion?
Women with a history of heavy or incredibly painful periods are at higher risk of expulsion. Postpartum women may also be at higher risk for expulsion.
If youve already had IUD expulsion then it is estimated that your risk of another is about fourteen percent.
What are the symptoms of expulsion?
More than the usual cramping, either with your period or outside of menses, can be a sign of expulsion. If you experience a significant increase in bleeding, continuous spotting, new vaginal discharge then youll want to see your doctor and possibly have a transvaginal ultrasound to check out where your IUD is currently residing.
Also Check: How Much Does Estradiol Cost
Theyre Safe For Teens And Women Who Havent Had Children
In the 1970s, IUDs had a very bad reputation. A device called the Dalkon Shield became infamous when it was found to have serious design flaws that made it unsuitable for adolescents and increased a womans risk of infection and infertility.
The IUDs of today are a world away from the Dalkon Shield. Considerable evidence suggests that Paragard, Mirena, Kyleena, Skyla, and Liletta are safe for most women, including teenagers, women who plan to become pregnant in the future, and women with multiple partners . The American College of Obstetricians and Gynecologists recommends IUDs as a safe, appropriate, and highly effective method of birth control for the majority of women.
Nexplanon Vs Mirena: Differences Similarities And Which Is Better For You
Drug overview & main differences | Conditions treated | Efficacy | Insurance coverage and cost comparison | Side effects | Drug interactions | Warnings | FAQ
When deciding on an effective and safe birth control method, you may be met with several options, such as birth control pills, birth control implants, and hormonal IUDs . The most effective options, however, are the etonogestrel contraceptive implant and the levonorgestrel intrauterine system . During the course of a year, fewer than 1 in 100 women will get pregnant while using an implant or intrauterine device.
Nexplanon and Mirena are non-pill forms of birth control that can help prevent pregnancy. Both drugs contain female hormone analogs called progestins. They do not contain estrogen.
Nexplanon is implanted under the skin of the upper arm while Mirena is an intrauterine device inserted into the uterus. They work by creating a hostile environment for sperm to prevent the fertilization of an egg. Progestins can also help stop the release of an egg from the ovaries . Continue reading to learn more about the similarities and differences between Nexplanon and Mirena.
Also Check: Blue Cross Blue Shield Testosterone Replacement Therapy
How Is It Taken Out
The hormonal IUD can stay in for 5 years but it can be taken out sooner. Your doctor or Family Planning NSW clinic can take it out. The clinician will remove the IUD by gently pulling on the string. This only takes a couple of minutes. Some people find it a little uncomfortable. If you want another hormonal IUD, the old one can be taken out and a new one put in at the same visit.
Coverage And Cost Comparison Of Nexplanon Vs Mirena
Many health insurance plans may help cover the cost of Nexplanon or Mirena. In general, Medicare plans do not provide coverage for birth control. Because no generic versions are available for Nexplanon or Mirena, costs can run high.
Contact your insurance provider or healthcare provider to determine the exact cost of Nexplanon or Mirena. A savings card from SingleCare may help lower the cost of Nexplanon and Mirena.
| Nexplanon |
| Yes | 6% |
Frequency is not based on data from a head-to-head trial. This may not be a complete list of adverse effects that can occur. Please refer to your doctor or healthcare provider to learn more.
Recommended Reading: Nugenix Estrogen Blocker
Thoughts On The Pros And Cons Of Hormonal Iuds
Loved this article!Ive had mirena for almost 7 years and I honestly love it. Its one of the best things Ive ever done for myself. I can see how it might not be the best option for some but for me, right now, it works.
Thank you for this article. Very informative. I currently have a Mirena IUD, my third, and I LOVE it and have never had one issue regarding it. However, due to my age, nearing 51, I am experiencing some pre menopausal symptoms I was wondering your thoughts on using an essential oil for the hormonal imbalance. Ive been reading about Young Livings Progessence Plus and it seems like it would be exactly what I need. Im just not sure if it would effect the iud at all. .Your thoughts??
I have had mirena for four years and I dont feel it untill a week before my period, I can feel where it is and it feels like dull stabbing and the pain goes down my leg a bit untill I do a hip flexor stretch, that seems to help, and also advil. Judging by what youre saying I would be weiry of putting anything in there. That cyst thing sounds terrible! And I dont think they recommend iuds for women with endometriosis.
Oops my bad I thought they were saying to not get an iud with endo but apparently it says it helps it. Well anyways like I said mine only bothers me about 4 days of the month and advil helps it quick. And not full days its like off and on but enough to need a pill.
How Long Does It Take For Mirena Hormones To Leave Your System
How long does it take for Mirena hormones to leave your system? Mirena works to thin the lining of your uterus to prevent the transport of sperm into your fallopian tubes where fertilization must occur. The progestin it releases also thickens your cervical mucus and can prevent ovulation. Mirena can last for up to five years after insertion.
How long does it take for IUD hormones to leave your body? When implanted, the IUD secretes a hormone much like progesterone known as levonorgestrel. Since the device is prescribed to stay put for five years, the womans body stops producing progesterone. According to Healthline, this happens because the womans body becomes dependent on the IUD.
How long after Mirena removal do hormones go back to normal? For some women, it can take three months after the IUD removal for your normal menstrual cycle to return. For most women, it returns almost immediately.
What happens to your body after IUD removal? You should feel completely normal after getting your IUD taken out. You may have some light bleeding after IUD removal, and some slight cramping during and right after removal. Any side effects that you may have had while you were on the IUD will eventually go away after your IUD is out.
Don’t Miss: Breakthrough Bleeding On Bioidentical Hormones
What Is Good About The Hormonal Iud
- It is an extremely effective method of contraception.
- Once inserted you will only need to check the string each month.
- It can last up to 5 years or longer if you have it inserted from 45 years of age.
- You can use it while breast feeding.
- No medications stop it from working.
- Most users have no vaginal bleeding at all or very light bleeding.
- Periods may be less painful.
- It can be taken out at any time by a doctor or nurse.
- Once removed your fertility quickly returns to what is normal for you.
- It is another contraceptive option if you have difficulty taking the hormone oestrogen. The Pill and vaginal ring contain oestrogen and progestogen. The hormonal IUD only contains progestogen.
What Happens If I Get Pregnant While I Am Using The Hormonal Iud
It is important that you see a doctor or nurse as soon as possible and have the IUD removed. The doctor or nurse will also need to rule out a pregnancy in your fallopian tubes . If the IUD is removed, you can continue the pregnancy or have an abortion. If the IUD cannot be removed and you continue the pregnancy, there is a higher risk of losing the pregnancy.
Also Check: Does Blue Cross Cover Testosterone Injections
Mirena As Contraception During Perimenopause
Anyone who has been using birth control to prevent pregnancy should continue to do so until they enter menopause.
While fertility typically starts to decline in a womanâs mid-30s, it is possible for some women to get pregnant into their 50s.
According to the standard definition, menopause has begun if 12 months have passed without a period. However, because the Mirena coil can stop periods from occurring, it is important to use another method of determining when menopause has begun.
A doctor may do a blood test to check for follicle-stimulating hormone and estrogen levels. During perimenopause, FSH levels typically rise as estrogen levels fall. The doctor may need to run the test more than once, since these levels can naturally fluctuate.
There is no set time to remove the Mirena coil, unless it expires.
Womenâs Health Concern recommend waiting for 1 year after the last period before stopping birth control.
Anyone who removes the Mirena coil before they enter menopause should switch to another form of birth control if they wish to prevent pregnancy.
Some people choose to wait until their coils expire, even after menopause has begun. A doctor can provide specific guidance.
Hormone replacement therapy can help alleviate some symptoms of menopause. It is not a form of birth control.
HRT injections, pills, or patches may ease some menopause symptoms, such as:
- night sweats
- lower bone density
- vaginal dryness
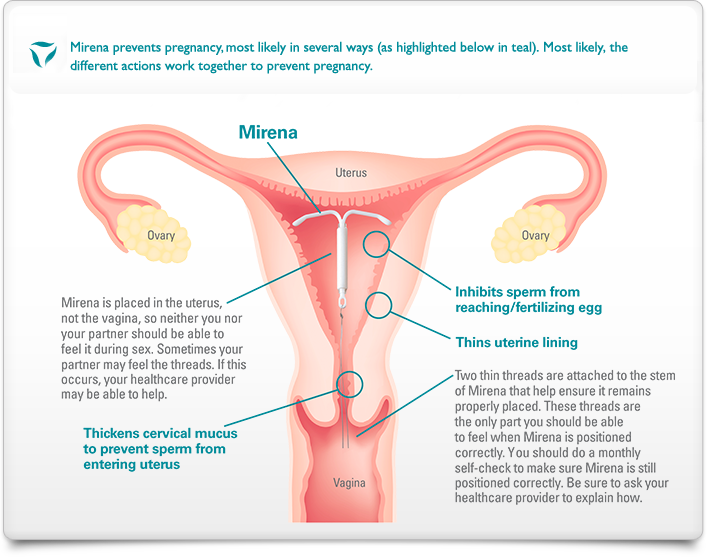
How Do They Work
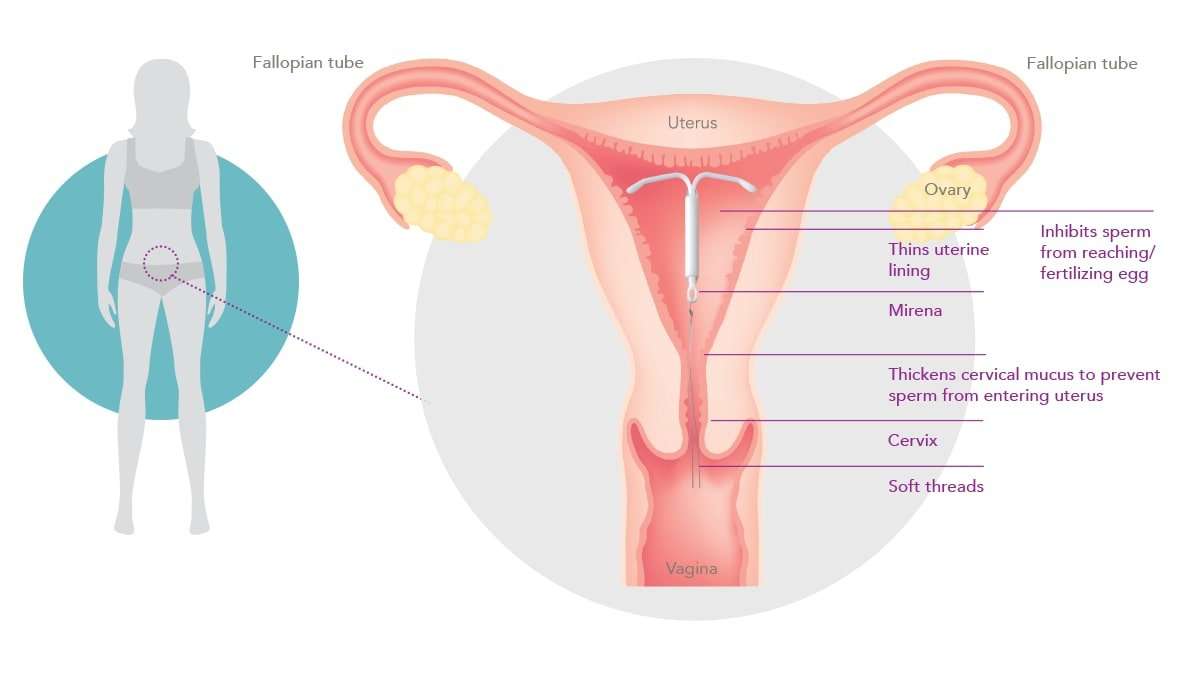
The IUD is placed inside the uterus by a doctor or nurse. The hormonal IUD:
- stops sperm from fertilising the egg
- makes the mucus in the cervix thicker so that sperm can’t get into the uterus
- changes the wall of the uterus, making it hard for an egg to attach to the wall
- sometimes stops your ovaries from releasing an egg
Don’t Miss: Does Blue Cross Blue Shield Cover Testosterone Treatment
Prerequisites To Use Mirena
Your doctor might not recommend you to get the Mirena inserted , if you have any of the following conditions-
- If you are currently a Breast cancer patient or had it in the past
- If you have Uterine or cervical cancer
- If you are experiencing any Liver related illness
- If you have abnormalities in the uterus, such as fibroids that might interfere in the placement or the retention of IUD
- If you are experiencing an infection in the pelvic region presently or a pelvic inflammatory disease
- If you are experiencing unexplained vaginal bleeding
What Is The Mirena Crash
There are reports of women experiencing short-term side effects after the removal of Mirena. While there is no concrete evidence on the cause of it, the Mirena crash may be associated with a temporary hormone imbalance after removal. Symptoms of Mirena crash may include headache, nausea, mood swings, insomnia, fatigue, and acne. These effects are usually temporary.
Don’t Miss: Microgestin And Hair Loss
Side Effects Of Mirena
For some women, the side effects seem like benefits. A lighter period for many women, and no period at all for 1 in 5 women with the Mirena IUD. But for other women, there may be troublesome, or even serious side effects.
Some women will experience a nearly endless period, with spotting or flow daily for weeks, to even months on end. If that happens, the best recommendation is to have the IUD removed. Other possible side effects include:
- Spotting between periods
- Development of ovarian cysts
- Severe side effects are rare, but include migration of the IUD out of place, perforation of the uterus, ectopic pregnancy, and increased risk of Pelvic Inflammatory Disease
The Most Knowledgeable People Are Using It
IUDs are the most popular choice for female health care providers who do counseling around family planning, such as obstetricians, gynecologists, midwives, and nurses. According to a study published in Obstetrics & Gynecology, of the health care providers surveyed who reported using contraception, 40 percent used IUDs. This contrasted with only 6.3 percent of women in the general population who used either an IUD or an implant .
Need help deciding if an IUD is right for you? Were available to talk through your options via phone or in person. Visit onemedical.com to contact your local One Medical office or to make an appointment.
Read Also: Zitsticka Skin Discipline Side Effects
Effects On The Symptoms Of Menopause
Menopause and perimenopause can cause various noticeable changes.
According to The Centre for Menstrual Cycle and Ovulation Research, about 25% of people entering into perimenopause experience heavy periods. This is due to significant fluctuations in hormone levels.
The Mirena coil can help lighten periods in people who experience heavy bleeding. Some find that this type of coil stops their periods altogether. If this occurs, it may be harder to know when menopause has begun.
However, because the Mirena coil contains no estrogen, it does not affect the symptoms of a reduction in estrogen as the body goes through menopause.
Meanwhile, the Mirena coil may cause additional symptoms during menopause because it contains progestogen, a version of the hormone progesterone.
This means that a person with a Mirena coil may experience symptoms such as:
How Does Mirena Work
Mirena birth control works by releasing levonorgestrel. This hormone thins the lining of the uterus. It also thickens the mucus in the cervix.
As a result, sperm has a hard time moving and surviving in the uterus. This prevents pregnancy.
The thinning of the uterine lining can also reduce or stop menstrual bleeding.
Also Check: How Much Is Estrogen Pills
What If I Am Using The Hormonal Iud And I Want To Become Pregnant
The hormonal IUD can be removed at any time by a trained doctor or a nurse. Your fertility will quickly return to what is normal for you.
Family Planning Victoria acknowledges the Aboriginal and Torres Strait Islander people as the Traditional Owners of the land on which our offices stand and in the regions in which we provide our services. We pay our respects to Elders past, present and future.
Family Planning Victoria is committed to providing respectful, inclusive services and work environments where all individuals feel accepted, safe, affirmed and celebrated. With our commitment to embracing diversity and eliminating all forms of discrimination in the provision of reproductive and sexual health services, we welcome all people irrespective of cultural or linguistic background, sexual orientation, gender identity, intersex status, religion or spiritual beliefs, socio economic status, age or abilities.
Pros Of Hormonal Iuds:
Unlike all other types of hormonal birth control, hormonal IUDs do not completely suppress ovulation . According to one study, Mirena suppresses ovulation in 85 percent of cycles during the first year , and then in 15 percent of cycles after that. Lower dose IUDs permit ovulation more of the time.
Compared to pills and implants, hormonal IUD delivers a lower dose of a contraceptive drug. The blood level of levonorgestrel in Mirena-users is about one-tenth of pill-users. Unfortunately, even that low dose can cause side effects .
Hormonal IUDs are more effective than almost any other method of contraception, with a failure rate of just 0.7 percent.
After insertion, you dont need to do anything or take anything, and IUDs lasts three years or five years .
In theory, fertility returns to normalalmost as soon as a hormonal IUD is removed.
Hormonal IUDs reduce menstrual flow by at least 90 percent, and thats a huge pro for heavy menstrual bleeding.
Hormonal IUDs can relieve some of the symptoms of endometriosis. For other endometriosis treatment ideas. .
You May Like: Nugenix Estro-regulator Review